Eiosinophilic Granuloma
Eiosinophilic Granuloma
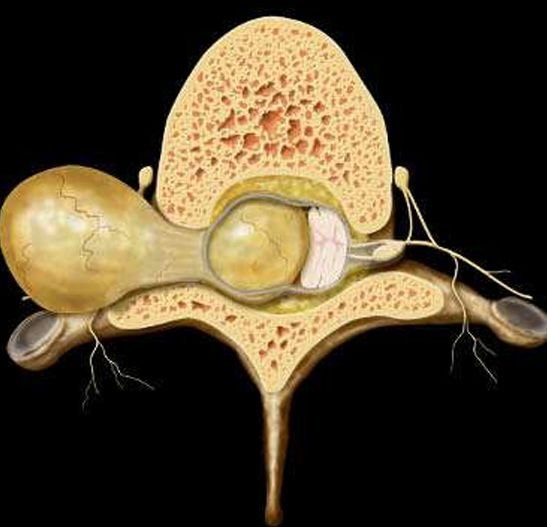
Pediatric spinal eosinophilic granuloma (EG) is a rare, benign bone lesion caused by Langerhans Cell Histiocytosis (LCH) that affects the vertebrae of the spine. Although it is a non-cancerous condition, spinal EG can result in vertebral collapse, instability, and spinal cord compression, which may lead to pain, deformity, or even neurological deficits in children. If not properly diagnosed and treated in time, this condition may severely impact a child’s growth, mobility, and quality of life. In Bangladesh, the rarity and diverse presentation of spinal EG often lead to misdiagnosis or delayed treatment, especially in rural settings. Dr. Md. Nafaur Rahman, one of the leading pediatric neurosurgeons in the country, offers expert evaluation and surgical care for children with spinal eosinophilic granuloma through both public (NINS) and private (BPNC) healthcare facilities. What is Spinal Eosinophilic Granuloma? Eosinophilic Granuloma (EG) is the most localized and benign form of Langerhans Cell Histiocytosis (LCH). It involves clonal proliferation of Langerhans cells, leading to destructive bone lesions. In pediatric patients, the spinal column is one of the most commonly affected skeletal sites. Key characteristics include: Typically affects the vertebral body, leading to collapse or “vertebra plana” Most common in the thoracic spine, followed by cervical and lumbar regions Occurs mainly in children aged 5–10 years Can present as an isolated lesion or part of multisystem disease Causes and Risk Factors Unknown cause, but associated with abnormal immune response Not inherited or contagious Some studies suggest environmental or viral triggers Can be part of systemic LCH, involving skin, lungs, or other bones Symptoms of Spinal EG in Children Children with spinal eosinophilic granuloma may present with: Localized back or neck pain Muscle spasm or stiffness Tenderness over the spine Restriction in spinal movement Postural abnormalities like scoliosis or kyphosis Neurological symptoms in advanced cases due to spinal cord compression, including: Limb weakness Numbness or tingling Difficulty walking Bowel/bladder dysfunction (rare) In Bangladesh, these symptoms are frequently mistaken for trauma, tuberculosis, or spondylitis, delaying proper treatment. Diagnosis in the Bangladeshi Context Timely diagnosis is essential to prevent permanent spinal damage. Clinical Evaluation Pain history, especially night pain Neurological examination Assessment of spinal deformity Family and past medical history to rule out systemic illness Imaging X-ray – may show vertebra plana or bony lytic lesion MRI – evaluates soft tissue involvement, cord compression, and edema CT scan – defines bony destruction and guides biopsy planning Bone scan / PET scan – in suspected multisystem LCH Biopsy – definitive diagnosis via histopathology and immunohistochemistry (CD1a+, Langerin+) Treatment Options Management of pediatric spinal EG depends on symptoms, spinal stability, and neurological involvement. Non-Surgical Management Observation and immobilization in asymptomatic or mildly symptomatic cases Bracing to support the spine Low-dose steroids or chemotherapy in multisystem disease Radiotherapy (rarely used in children due to long-term risks) Surgical Management by Dr. Nafaur Rahman Surgery is indicated in: Progressive neurological symptoms Spinal instability Spinal deformity Failure of conservative treatment Surgical Approaches: Biopsy and decompression to relieve spinal cord pressure Tumor excision if safe and feasible Spinal fusion or instrumentation in cases with instability or collapse Minimally invasive techniques when appropriate Postoperative Recovery and Prognosis Most children recover well with timely intervention Pain and neurological symptoms often resolve quickly Physical therapy improves mobility and function Regular follow-up imaging to monitor for recurrence Prognosis is excellent in solitary EG, though systemic LCH may require long-term treatment Challenges in Bangladesh Misdiagnosis as tuberculosis or general spinal infection Limited access to pediatric spine MRI in rural districts Lack of specialized pediatric neurosurgical care outside Dhaka Low awareness among general physicians and orthopedists Financial barriers delaying diagnosis and surgery Why Choose Dr. Md. Nafaur Rahman? Pioneer in pediatric spinal tumor diagnosis and surgery in Bangladesh Offers evidence-based, child-friendly care in both government and private settings Uses modern surgical techniques, including microsurgery and image guidance Operates in NINS (public) and Bangladesh Paediatric Neurocare Centre (private) Committed to early intervention, better outcomes, and child-centered rehabilitation Works with a multidisciplinary team for accurate diagnosis and comprehensive care Appointment & Contact Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Appointment/Serial: 📱 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com