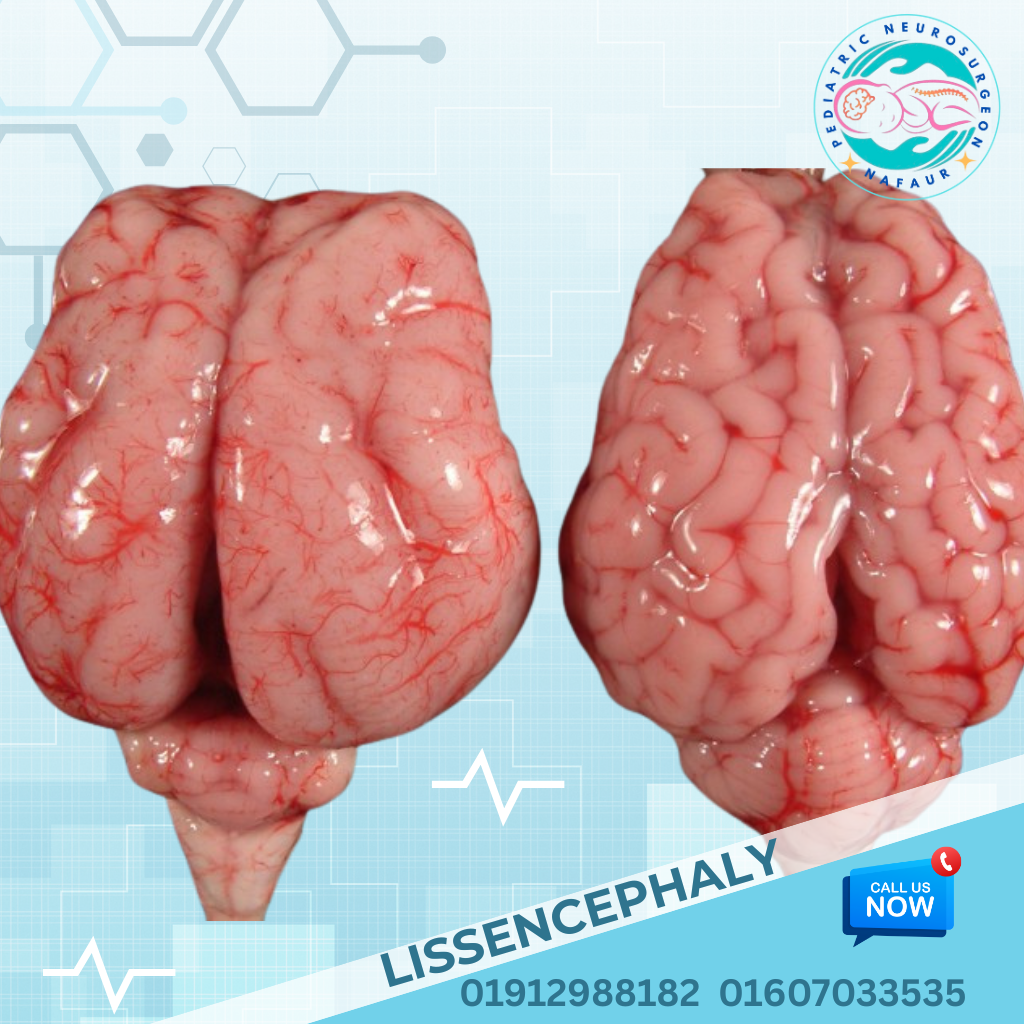
Lissencephaly
Lissencephaly
Lissencephaly, meaning “smooth brain,” is a rare congenital brain malformation caused by impaired neuronal migration during early fetal development. It results in a lack of normal brain folds (gyri) and grooves (sulci), leading to a smooth appearance of the cerebral cortex. Lissencephaly can be complete or partial, and is often associated with developmental delay, seizures, feeding difficulties, and muscle tone abnormalities. This disorder is typically diagnosed in infancy, though severe forms may be identified prenatally. It is one of the most debilitating pediatric neurological conditions, requiring lifelong medical and supportive care. 🌍 Lissencephaly in Bangladesh In Bangladesh, many cases of lissencephaly are diagnosed late, often after the child presents with intractable seizures, failure to meet milestones, or unexplained hypotonia. Due to lack of awareness and limited availability of prenatal MRI in rural areas, early detection is uncommon. However, with improved neuroimaging facilities and expert pediatric neurosurgical care at NINS and the Bangladesh Paediatric Neurocare Centre, early diagnosis and supportive management are now more accessible. 🧠 Types of Lissencephaly Lissencephaly is classified based on the appearance of the brain surface and genetic mutation involved: Type I (Classic Lissencephaly): Smooth cortex due to complete or nearly complete absence of gyri Often caused by mutations in LIS1, DCX genes Type II (Cobblestone Lissencephaly): Bumpy or cobblestone-like cortex, associated with congenital muscular dystrophies (e.g., Walker-Warburg syndrome) Severity varies: Agyria: Complete absence of gyri Pachygyria: Broad, reduced gyri Subcortical Band Heterotopia (SBH): Abnormal gray matter layers beneath the cortex, often in females with DCX mutation ⚠️ Causes and Risk Factors Genetic mutations: LIS1, DCX, ARX, RELN, and others X-linked inheritance in some cases (more severe in boys) Prenatal infections such as CMV, toxoplasmosis Maternal diabetes, toxic exposures, or ischemic injury during early gestation Idiopathic in some children with no known family history 🧒 Symptoms and Clinical Features Symptoms typically begin in the first few months of life, and may include: Developmental delay and intellectual disability Seizures, often early-onset and drug-resistant (e.g., infantile spasms) Poor feeding and failure to thrive Muscle tone abnormalities – hypotonia or spasticity Microcephaly (small head size) or occasionally macrocephaly Visual impairment and nystagmus Swallowing difficulties, drooling Breathing abnormalities in severe cases 🔍 Diagnosis and Imaging Accurate diagnosis involves neuroimaging and genetic testing: 1. MRI Brain Gold standard: reveals absence of normal gyral patterns Shows thickened cortex, broad or absent sulci, and abnormal white matter structure Can help classify agyria, pachygyria, and SBH 2. EEG Identifies seizure activity and type of epilepsy Often shows hypsarrhythmia in infantile spasms 3. Genetic Testing Confirms mutation in LIS1, DCX, ARX, or other genes Important for family counseling and future pregnancies 4. Prenatal Diagnosis Second-trimester ultrasound or fetal MRI may reveal abnormal brain development Still limited in Bangladesh but growing in tertiary centers 🛠️ Treatment and Neurosurgical Considerations There is no cure for lissencephaly, but neurosurgical and supportive care can help manage complications and improve quality of life. 1. Seizure Management Anti-epileptic drugs (AEDs): valproate, levetiracetam, topiramate Intractable epilepsy may require palliative neurosurgical options: Vagus nerve stimulation (VNS) Corpus callosotomy Focal resection in SBH cases with localized seizures 2. Hydrocephalus or Increased ICP In rare cases with associated hydrocephalus, VP shunt surgery may be needed 3. Feeding Support Gastrostomy tube placement in children with severe dysphagia 4. Rehabilitation Physiotherapy, occupational therapy, and speech therapy are essential Early intervention improves motor, sensory, and communication abilities 5. Family Counseling Ongoing support and genetic counseling for affected families 🔄 Prognosis Prognosis depends on the type and severity of the lissencephaly Children with agyria or extensive pachygyria often have profound intellectual and physical disabilities Refractory seizures are a major cause of complications Lifelong care is required with a multidisciplinary team including neurologists, therapists, and neurosurgeons With proper management, some children can achieve developmental milestones and improved quality of life 👨⚕️ Why Choose Dr. Md. Nafaur Rahman? One of Bangladesh's leading experts in congenital brain malformations and pediatric epilepsy surgery Specialized in advanced MRI interpretation, surgical planning, and long-term neurodevelopmental care Operates at National Institute of Neurosciences & Hospital (NINS) – the premier referral center for pediatric neurosurgery Provides family-centered care, counseling, and access to modern interventions Offers coordination with genetic counselors and neurorehabilitation teams 📞 Get Expert Guidance for Your Child Dr. Md. Nafaur Rahman Assistant Professor, Department of Pediatric Neurosurgery, NINS Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Call for Appointment: 01912988182 | 01607033535 🌐 Visit: www.neurosurgeonnafaur.com