Chordomas
Chordomas
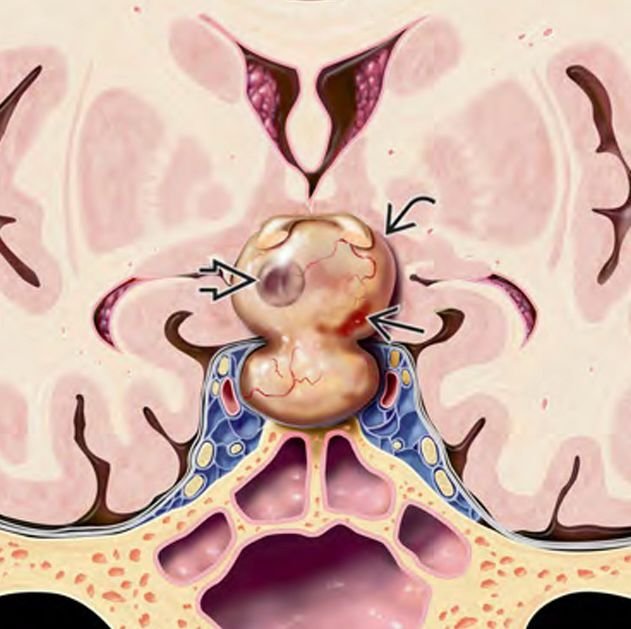
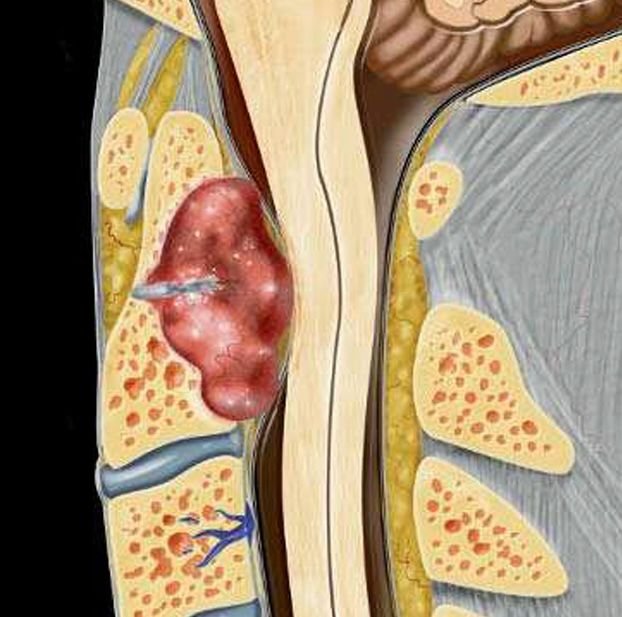
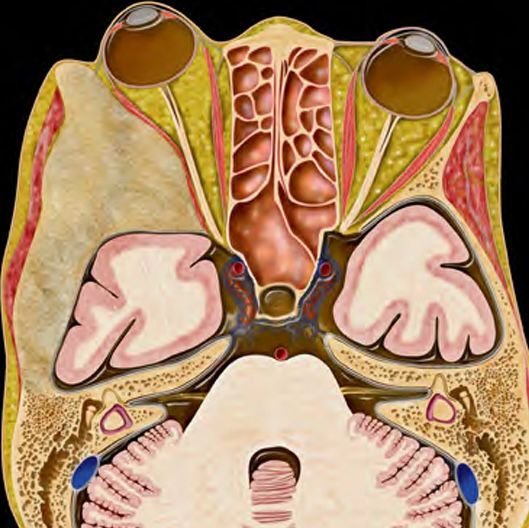
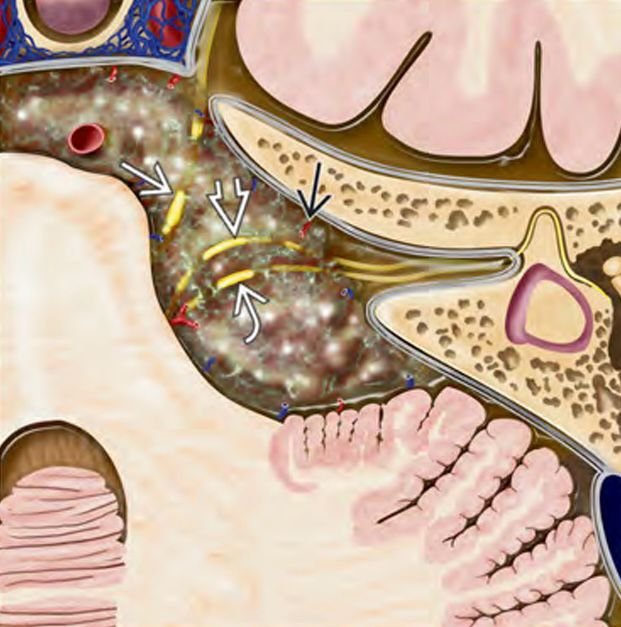
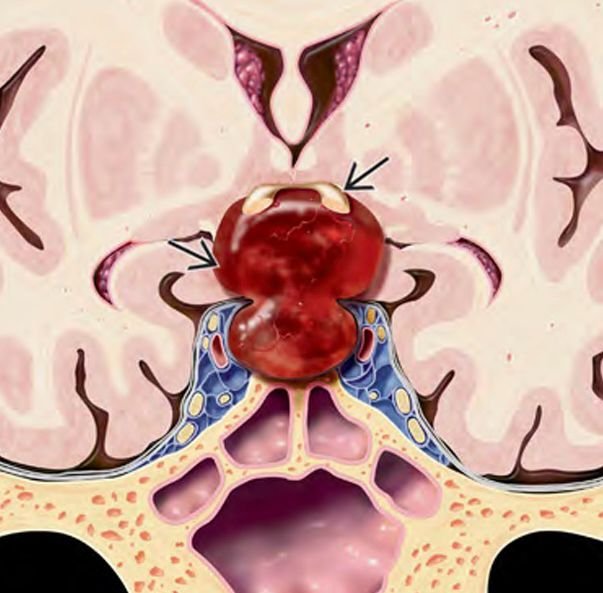
Chordomas are rare, slow-growing but locally aggressive tumors that arise from embryonic remnants of the notochord. In children, skull base chordomas typically occur at the clivus, a bone located at the junction of the brain and spine, making surgical access complex and challenging. Despite being histologically benign, chordomas can behave malignantly by compressing vital neurovascular structures. Pediatric chordomas are particularly challenging due to their deep location, infiltrative nature, and recurrence risk. These tumors require expert-level neurosurgical intervention, ideally by a pediatric neurosurgeon trained in skull base techniques. In Bangladesh, Dr. Md. Nafaur Rahman is one of the few specialists offering complete care for such complex cases, including advanced imaging, precision surgery, and long-term follow-up. 🌍 Skull Base Chordomas in Bangladesh – Challenges in Early Diagnosis In Bangladesh, most children with clival chordomas present late due to lack of access to high-resolution MRI, delays in referral, or misinterpretation of early symptoms such as headache, nasal obstruction, or diplopia (double vision). These signs are often mistaken for sinusitis, vision problems, or ENT disorders. As a result, children may only reach a neurosurgeon once the tumor has grown substantially and begun compressing the brainstem, optic nerves, or cranial nerves. Early diagnosis and referral to experienced centers like NINS or Bangladesh Paediatric Neurocare Centre are critical for improving outcomes. 🧬 Pathology and Classification Origin: Remnants of the notochord, an embryonic midline structure Common Location: Clivus in the skull base in pediatric cases WHO Classification: Generally low-grade (Grade I), but locally aggressive Histology: Lobulated masses with physaliphorous (bubbly) cells and mucinous matrix Can infiltrate bone, brainstem, cavernous sinus, and cranial nerves 🧒 Symptoms of Skull Base Chordomas in Children Persistent headache, especially at the back or center of the head Double vision (diplopia) or difficulty moving eyes (cranial nerve palsy) Facial numbness or weakness Nasal blockage or discharge if the tumor invades nasal cavity Neck stiffness or pain Difficulty swallowing or hoarseness Balance problems or unsteady gait Growth delay or hormonal changes (if the pituitary gland is involved) 🔍 Diagnosis of Pediatric Skull Base Chordomas 🧠 Imaging Studies MRI with contrast: Essential to determine tumor extent and relation to brainstem, cranial nerves, and vessels CT Scan: Shows bony erosion of clivus MRI Spine: To rule out drop metastases (rare) 🧪 Histopathology Confirmed via biopsy or post-surgical specimen Positive for cytokeratin, EMA, S100, and brachyury markers Helps differentiate from chondrosarcoma and other skull base tumors 🛠️ Treatment Options ✂️ Surgical Resection The cornerstone of treatment Aim is maximal safe resection without damaging brainstem or cranial nerves Transnasal endoscopic approach or open skull base surgery used based on size/location Dr. Nafaur Rahman uses advanced tools such as neuro-navigation, intraoperative monitoring, and endoscopic assistance to improve precision 🔬 Radiotherapy Required in most cases after surgery to reduce recurrence Proton beam therapy preferred internationally, but intensity-modulated radiotherapy (IMRT) used in Bangladesh Should be tailored based on child’s age, tumor residual, and extent 💊 Chemotherapy Not standard; used only in select aggressive or recurrent cases 🔄 Prognosis and Long-term Outlook Recurrence rate is high, hence long-term follow-up is essential Prognosis improves significantly with early diagnosis, skilled resection, and appropriate radiotherapy Many children lead normal or near-normal lives with multidisciplinary management Regular MRI monitoring (every 6–12 months) for at least 5–10 years ⚠️ Delayed Diagnosis – Consequences in Bangladesh Brainstem compression leading to life-threatening complications Vision loss or cranial nerve palsy Infiltration of vital blood vessels, making surgery difficult Tumor recurrence due to incomplete resection Psychological stress on families and academic disruption 👨⚕️ Why Dr. Md. Nafaur Rahman? One of the few pediatric neurosurgeons in Bangladesh with expertise in skull base chordoma surgery Uses advanced technologies like neuro-navigation, intraoperative imaging, and endoscopic approaches Collaborates with oncologists, ENT surgeons, and radiation oncologists for comprehensive care Offers affordable and accessible services through NINS and Bangladesh Paediatric Neurocare Centre 📞 Contact for Expert Consultation Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial & Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com