Chondrosarcomas
Chondrosarcomas
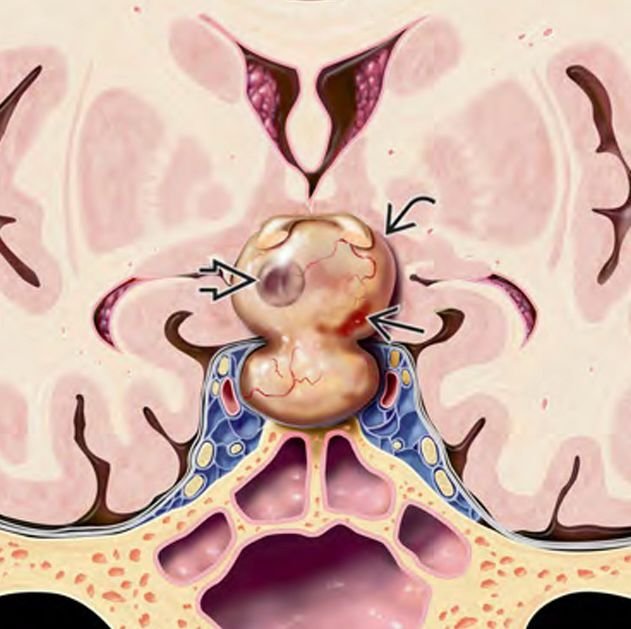
Chondrosarcomas are malignant tumors that originate from cartilage-producing cells and can develop at the skull base, particularly in areas like the petroclival junction, sphenoid bone, and occipital clivus. Although more common in adults, skull base chondrosarcomas in children are rare but aggressive, and their proximity to cranial nerves, brainstem, and major blood vessels makes them particularly challenging to manage. These tumors often grow slowly but can invade bone and critical neurovascular structures, causing neurological deficits. They require precise imaging, expert neurosurgical excision, and often adjuvant radiotherapy for optimal outcomes. In Bangladesh, early diagnosis and referral to specialized centers like NINS or Bangladesh Paediatric Neurocare Centre under the care of Dr. Md. Nafaur Rahman can significantly improve treatment outcomes. 🌍 Skull Base Chondrosarcoma in Bangladesh – The Need for Specialized Care In Bangladesh, pediatric patients with skull base chondrosarcomas often face delays in diagnosis due to: Misattribution of symptoms to ENT or ophthalmologic conditions Limited availability of MRI with skull base protocol Lack of multidisciplinary tumor boards in many general hospitals Dr. Md. Nafaur Rahman provides skull base tumor diagnostics, microsurgical & endoscopic surgical intervention, and collaborative oncologic care, tailored specifically for children with rare skull base neoplasms. 🧬 Tumor Characteristics Origin: Mesenchymal cells producing cartilage Common Locations: Petroclival synchondrosis, spheno-occipital junction, jugular foramen Histologic Types: Conventional, mesenchymal (more aggressive in children) WHO Grading: Grade I–III based on mitotic activity and cellular atypia Differential Diagnosis: Skull base chordomas, osteosarcomas, Ewing’s sarcoma, meningiomas 🧒 Clinical Symptoms in Children Symptoms depend on tumor size and location. Often subtle in early stages, common signs include: Persistent headaches Diplopia (double vision) due to cranial nerve VI involvement Facial numbness or weakness (cranial nerves V and VII) Hearing loss or tinnitus Swallowing difficulty, hoarseness (lower cranial nerve involvement) Balance issues or unsteady gait Hydrocephalus if brainstem or ventricular system is compressed Nasal obstruction or nosebleeds (rare anterior tumors) 🔍 Diagnostic Approach 🧠 Imaging MRI with contrast (preferred): Shows lobulated, enhancing lesion with bone involvement CT scan: Highlights bony destruction and calcifications MR Angiography: Useful for assessing vascular encasement Whole spine MRI: In aggressive cases to rule out drop metastases 🔬 Biopsy & Histopathology Necessary for definitive diagnosis Shows cartilaginous matrix with atypical chondrocytes Immunohistochemistry: S100, SOX9 positive; Ki-67 helps grade aggressiveness 🛠️ Treatment Strategies ✂️ Surgical Resection Mainstay of treatment Goal: Maximal safe resection while preserving cranial nerve function Approach depends on tumor location: Endoscopic endonasal for anterior skull base Retrosigmoid/suboccipital for posterior skull base Transpetrosal or combined approaches for complex petroclival lesions Dr. Nafaur Rahman employs advanced tools like neuro-navigation, endoscopy, and intraoperative neuromonitoring to minimize morbidity ☢️ Radiotherapy Indicated in incomplete resections or high-grade tumors Proton beam therapy (preferred internationally, limited in Bangladesh) Stereotactic radiosurgery (SRS) or IMRT used locally when needed 💊 Chemotherapy Rarely effective in chondrosarcoma; used only in mesenchymal variant or metastatic disease 🔄 Prognosis Depends on: Tumor grade and location Extent of surgical removal Availability of precision radiotherapy Grade I tumors have favorable outcomes with surgery alone Higher-grade or recurrent tumors require long-term monitoring and multimodal therapy 5-year survival: ~70–90% for low-grade, ~30–50% for high-grade tumors Regular MRI every 6–12 months essential for recurrence surveillance ⚠️ Why Early Diagnosis Matters Delays in recognition and treatment can lead to: Permanent cranial nerve deficits (e.g., facial palsy, hearing loss) Brainstem compression and hydrocephalus Tumor invasion of critical arteries (e.g., basilar artery) Compromised surgical outcomes due to tumor spread 👨⚕️ Why Choose Dr. Md. Nafaur Rahman? Leading authority on complex pediatric skull base tumor surgery in Bangladesh Pioneer in minimally invasive endoscopic and open approaches for difficult tumors Access to multidisciplinary neuro-oncology care at NINS Offers affordable, ethical, and evidence-based treatment protocols for rare brain tumors Long-term follow-up and support services through Bangladesh Paediatric Neurocare Centre 📞 For Consultation & Serial Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial & Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com