Langerhans Cell Histiocytosis
Langerhans Cell Histiocytosis
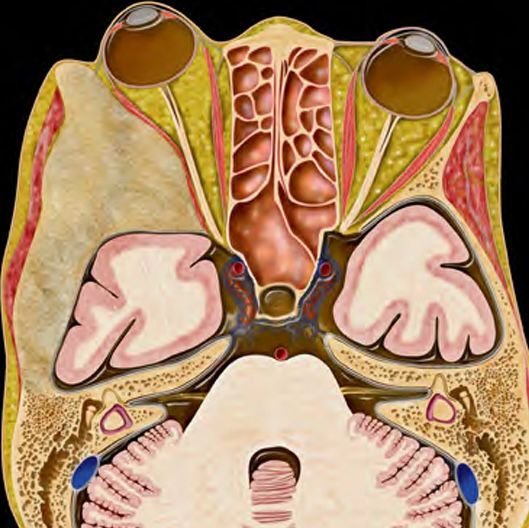
Langerhans Cell Histiocytosis (LCH) is a rare disorder in children characterized by the abnormal accumulation of Langerhans cells, a type of immune cell, which can form tumors or inflammatory lesions in various parts of the body. While LCH can affect organs like the skin, lungs, liver, and bones, one of the more serious manifestations includes involvement of the skull and central nervous system (CNS), requiring expert pediatric neurosurgical evaluation and management. In Bangladesh, LCH is often underdiagnosed or misdiagnosed due to its rarity and nonspecific symptoms. At the forefront of pediatric neuro-oncology in the country, Dr. Md. Nafaur Rahman leads a specialized team offering accurate diagnosis, multidisciplinary management, and advanced surgical care for children suffering from skull and CNS involvement of LCH. What is Langerhans Cell Histiocytosis? LCH is a disease where immature dendritic cells (Langerhans cells) proliferate abnormally and infiltrate various tissues. Though considered a rare disease, it has features of both inflammation and cancer. In children, bone lesions, especially in the skull, are the most common presentation. It may be classified as: Single-System LCH: Involves one organ or system (e.g., skull bone) Multisystem LCH: Involves multiple organs (e.g., bone + skin or brain + liver) CNS-Risk LCH: Involves craniofacial bones or direct brain infiltration Prevalence in Bangladesh While exact national data is limited, pediatric cases of LCH in Bangladesh are increasingly reported due to improved imaging and biopsy capabilities. However, lack of awareness among general practitioners and pediatricians means that many cases, especially with skull bone involvement, are wrongly diagnosed as simple infections or trauma-related lesions. Children may receive antibiotics for months without improvement. Common Symptoms in Children LCH may present with varying symptoms depending on the site of involvement: When the Skull is Affected: Hard or soft lump on the scalp, often in the frontal or parietal region Localized pain or tenderness over the lesion Swelling that does not respond to antibiotics Bone erosion visible on X-ray or CT scan Occasionally, discharge from the scalp or signs of infection When the Brain is Involved: Seizures or neurological deficits Behavioral or cognitive changes Signs of increased intracranial pressure Diabetes insipidus due to pituitary involvement Diagnostic Approach Early diagnosis is essential for preventing complications and planning appropriate treatment. Dr. Nafaur Rahman follows an evidence-based, child-friendly diagnostic protocol: 1. Imaging X-ray Skull: Often shows punched-out bone lesions CT Scan: Helps assess bony destruction and intracranial extension MRI Brain: Critical for detecting CNS involvement, pituitary dysfunction, or meningeal lesions 2. Biopsy Open or needle biopsy of the lesion is essential to confirm LCH Histopathological examination shows Langerhans cells Immunohistochemistry (CD1a and Langerin positive) confirms diagnosis 3. Systemic Evaluation PET scan or bone scan to detect other skeletal lesions Blood tests, liver function, and endocrine screening for systemic involvement Treatment Options Management of LCH in children requires a multidisciplinary team, including pediatric neurosurgeons, oncologists, and endocrinologists. Dr. Nafaur Rahman ensures all aspects are addressed under one coordinated care model. A. Surgical Management Indicated in isolated skull lesions or those causing mass effect Complete excision of the lesion with bone reconstruction if needed Surgery is often curative in single-system skull LCH Biopsy for diagnosis when multisystem disease is suspected B. Medical Management Steroid therapy for inflammation control Chemotherapy in multisystem or recurrent cases (vinblastine, cytarabine, etc.) Radiation therapy in select cases (very rare in children) C. Endocrinologic Support Children with pituitary involvement may need hormone replacement therapy Diabetes insipidus management is crucial in CNS-risk cases Outcomes and Prognosis Excellent prognosis in single-system, surgically treated cases Multisystem cases require long-term follow-up and therapy Recurrence is possible, especially if incompletely excised or part of systemic disease Early diagnosis and treatment greatly improve survival and quality of life Challenges in Bangladesh Misdiagnosis as scalp abscess, infection, or trauma Delayed referral to pediatric neurosurgical centers Limited access to biopsy and immunohistochemistry in rural areas Financial constraints in long-term follow-up and imaging Why Choose Dr. Md. Nafaur Rahman? Extensive experience with rare pediatric skull and CNS lesions Performs safe, minimally invasive surgery with a focus on bone preservation and cosmetic reconstruction Access to modern diagnostics including MRI, CT, and biopsy services Collaborates with pediatric oncologists and endocrinologists for complete care Trusted by hundreds of families for ethical, transparent, and expert care Contact for Appointment Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Serial/Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com