Scalp and Skull Neoplasms
Scalp and skull neoplasms in children are a diverse group of tumors that arise from the skin, subcutaneous tissue, bone (calvaria), or even from embryonic remnants. These tumors may be benign or malignant, and although they often appear as painless swellings, some can be locally aggressive or extend into the brain.
In Bangladesh, due to lack of awareness, delayed presentation, and limited pediatric neurosurgical access, many children with scalp or skull masses are misdiagnosed or inadequately treated. At NINS and Bangladesh Paediatric Neurocare Centre, Dr. Md. Nafaur Rahman offers state-of-the-art evaluation, surgical treatment, and long-term follow-up for these rare but important conditions.
 Types of Scalp and Skull Tumors in Children
Pediatric scalp and skull neoplasms can be classified based on origin:
1. Congenital Lesions
Dermoid and Epidermoid Cysts – Commonly seen near the midline; may contain hair or skin elements
Encephaloceles – Herniation of brain tissue through a skull defect (requires urgent surgery)
Sinus Pericranii – Abnormal venous connection between brain and scalp
Vascular Malformations (e.g., hemangiomas, AVMs)
2. Benign Neoplasms
Osteomas – Dense bony growths
Langerhans Cell Histiocytosis (LCH) – Can present as solitary or multiple skull lesions
Fibrous Dysplasia – Abnormal bone development often involving the skull
Lipomas – Fatty masses in the scalp
Neurofibromas – Associated with Neurofibromatosis Type 1 (NF1)
3. Malignant Tumors
Ewing’s Sarcoma – Aggressive bone tumor; requires combined treatment
Rhabdomyosarcoma – Affects soft tissue of scalp and orbit
Metastatic Lesions – Rare in children, but possible from neuroblastoma or leukemia
Primitive Neuroectodermal Tumors (PNETs) – Highly malignant, needs urgent treatment
Types of Scalp and Skull Tumors in Children
Pediatric scalp and skull neoplasms can be classified based on origin:
1. Congenital Lesions
Dermoid and Epidermoid Cysts – Commonly seen near the midline; may contain hair or skin elements
Encephaloceles – Herniation of brain tissue through a skull defect (requires urgent surgery)
Sinus Pericranii – Abnormal venous connection between brain and scalp
Vascular Malformations (e.g., hemangiomas, AVMs)
2. Benign Neoplasms
Osteomas – Dense bony growths
Langerhans Cell Histiocytosis (LCH) – Can present as solitary or multiple skull lesions
Fibrous Dysplasia – Abnormal bone development often involving the skull
Lipomas – Fatty masses in the scalp
Neurofibromas – Associated with Neurofibromatosis Type 1 (NF1)
3. Malignant Tumors
Ewing’s Sarcoma – Aggressive bone tumor; requires combined treatment
Rhabdomyosarcoma – Affects soft tissue of scalp and orbit
Metastatic Lesions – Rare in children, but possible from neuroblastoma or leukemia
Primitive Neuroectodermal Tumors (PNETs) – Highly malignant, needs urgent treatment
 Clinical Features of Scalp and Skull Tumors
Early detection can be life-saving. Parents should watch for:
Painless lump on the scalp or skull
Rapid increase in size
Discoloration or ulceration of skin over the lump
Bone deformity or asymmetry of skull
Headache, vomiting, or seizures (if there is brain involvement)
Signs of raised intracranial pressure
Neurological deficits or irritability in infants
In Bangladesh, such lumps are sometimes dismissed as birth marks or “fatty tumors” by local practitioners, leading to late intervention.
Clinical Features of Scalp and Skull Tumors
Early detection can be life-saving. Parents should watch for:
Painless lump on the scalp or skull
Rapid increase in size
Discoloration or ulceration of skin over the lump
Bone deformity or asymmetry of skull
Headache, vomiting, or seizures (if there is brain involvement)
Signs of raised intracranial pressure
Neurological deficits or irritability in infants
In Bangladesh, such lumps are sometimes dismissed as birth marks or “fatty tumors” by local practitioners, leading to late intervention.
 Diagnosis and Evaluation
A thorough evaluation is essential to differentiate between benign and malignant, intra- and extracranial, or vascular and solid lesions. At Dr. Nafaur’s centers, the work-up includes:
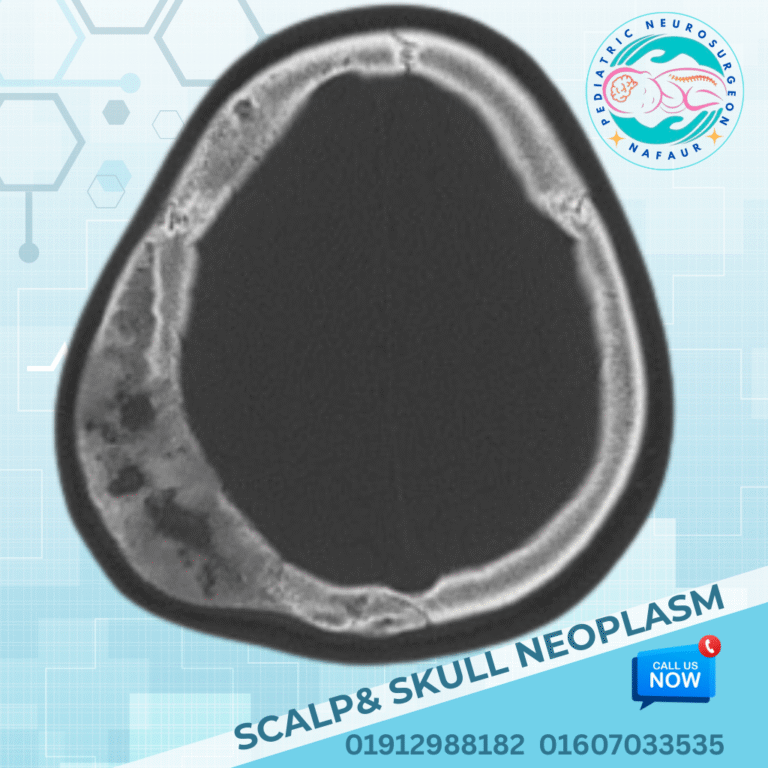
MRI Brain & Skull with Contrast – Identifies tumor extension, brain involvement, and precise anatomy
CT Scan with 3D Skull Reconstruction – Useful for bone tumors and surgical planning
Ultrasound (USG) – For superficial scalp lesions in infants
Biopsy or FNAC – For histological diagnosis in selected cases
Blood tests – To rule out systemic disease or infection
Tumor markers – If malignancy is suspected
All investigations are available at NINS and BP Neurocare Centre, under the direct care of Dr. Md. Nafaur Rahman.
Diagnosis and Evaluation
A thorough evaluation is essential to differentiate between benign and malignant, intra- and extracranial, or vascular and solid lesions. At Dr. Nafaur’s centers, the work-up includes:
MRI Brain & Skull with Contrast – Identifies tumor extension, brain involvement, and precise anatomy
CT Scan with 3D Skull Reconstruction – Useful for bone tumors and surgical planning
Ultrasound (USG) – For superficial scalp lesions in infants
Biopsy or FNAC – For histological diagnosis in selected cases
Blood tests – To rule out systemic disease or infection
Tumor markers – If malignancy is suspected
All investigations are available at NINS and BP Neurocare Centre, under the direct care of Dr. Md. Nafaur Rahman.
 Surgical Treatment of Scalp and Skull Tumors
The mainstay of treatment for most scalp and skull tumors is surgical excision. Surgery can be curative, diagnostic, or palliative, depending on the type and location of the lesion.
Surgical Goals:
Complete tumor removal
Preserve underlying brain and vital structures
Reconstruct the skull defect (cranioplasty) if needed
Minimize scarring and cosmetic deformity
Surgical Techniques:
Minimally invasive excision for superficial lesions
Craniotomy with skull reconstruction for deep or bone-invasive tumors
Image-guided surgery using neuronavigation
Multidisciplinary approach with plastic and reconstructive surgeons when needed
Endoscopic assistance for certain midline or intradural lesions
“Each child’s skull and scalp anatomy is unique. In pediatric neurosurgery, surgical finesse is as important as complete tumor removal.”
— Dr. Md. Nafaur Rahman
Surgical Treatment of Scalp and Skull Tumors
The mainstay of treatment for most scalp and skull tumors is surgical excision. Surgery can be curative, diagnostic, or palliative, depending on the type and location of the lesion.
Surgical Goals:
Complete tumor removal
Preserve underlying brain and vital structures
Reconstruct the skull defect (cranioplasty) if needed
Minimize scarring and cosmetic deformity
Surgical Techniques:
Minimally invasive excision for superficial lesions
Craniotomy with skull reconstruction for deep or bone-invasive tumors
Image-guided surgery using neuronavigation
Multidisciplinary approach with plastic and reconstructive surgeons when needed
Endoscopic assistance for certain midline or intradural lesions
“Each child’s skull and scalp anatomy is unique. In pediatric neurosurgery, surgical finesse is as important as complete tumor removal.”
— Dr. Md. Nafaur Rahman
 Adjuvant Therapy & Follow-Up
Radiotherapy or chemotherapy may be needed for malignant tumors like Ewing’s sarcoma or rhabdomyosarcoma.
Regular MRI or CT scans are essential for early detection of recurrence.
Psychosocial support and cosmetic rehabilitation are provided as needed.
Long-term monitoring of growth and skull development, especially if cranioplasty was done.
Adjuvant Therapy & Follow-Up
Radiotherapy or chemotherapy may be needed for malignant tumors like Ewing’s sarcoma or rhabdomyosarcoma.
Regular MRI or CT scans are essential for early detection of recurrence.
Psychosocial support and cosmetic rehabilitation are provided as needed.
Long-term monitoring of growth and skull development, especially if cranioplasty was done.
 Bangladesh Perspective: Need for Early Detection & Access
Despite being surgically treatable, many scalp and skull tumors in Bangladeshi children are missed, misdiagnosed, or poorly managed, leading to preventable complications.
Challenges include:
Lack of awareness among general physicians
Limited pediatric neurosurgical services outside major cities
Delay in performing MRI or CT due to cost
Misinterpretation of tumors as abscesses or “birthmarks”
Dr. Md. Nafaur Rahman is committed to overcoming these barriers by offering:
Affordable, expert care
Parental counseling and education
Timely surgery using the latest techniques
Coordination with pediatric oncology and reconstructive surgery units
Bangladesh Perspective: Need for Early Detection & Access
Despite being surgically treatable, many scalp and skull tumors in Bangladeshi children are missed, misdiagnosed, or poorly managed, leading to preventable complications.
Challenges include:
Lack of awareness among general physicians
Limited pediatric neurosurgical services outside major cities
Delay in performing MRI or CT due to cost
Misinterpretation of tumors as abscesses or “birthmarks”
Dr. Md. Nafaur Rahman is committed to overcoming these barriers by offering:
Affordable, expert care
Parental counseling and education
Timely surgery using the latest techniques
Coordination with pediatric oncology and reconstructive surgery units
 Why Trust Dr. Md. Nafaur Rahman?
Why Trust Dr. Md. Nafaur Rahman?
 Renowned pediatric neurosurgeon with special interest in scalp/skull tumors
Renowned pediatric neurosurgeon with special interest in scalp/skull tumors
 Operates at NINS, Bangladesh’s top neurosurgical institute
Operates at NINS, Bangladesh’s top neurosurgical institute
 Uses advanced tools including navigation and endoscopy
Uses advanced tools including navigation and endoscopy
 Skilled in cosmetic reconstruction of skull and scalp defects
Skilled in cosmetic reconstruction of skull and scalp defects
 Dedicated to providing Bangladesh’s children with world-class neurosurgical care
Dedicated to providing Bangladesh’s children with world-class neurosurgical care
 Contact for Pediatric Skull and Scalp Tumor Consultation
Dr. Md. Nafaur Rahman
Assistant Professor, Pediatric Neurosurgery, NINS
Chief Consultant, Bangladesh Paediatric Neurocare Centre
Contact for Pediatric Skull and Scalp Tumor Consultation
Dr. Md. Nafaur Rahman
Assistant Professor, Pediatric Neurosurgery, NINS
Chief Consultant, Bangladesh Paediatric Neurocare Centre
 For Serial/Appointment: 01912988182 | 01607033535
For Serial/Appointment: 01912988182 | 01607033535
 Website: www.neurosurgeonnafaur.com
Website: www.neurosurgeonnafaur.com