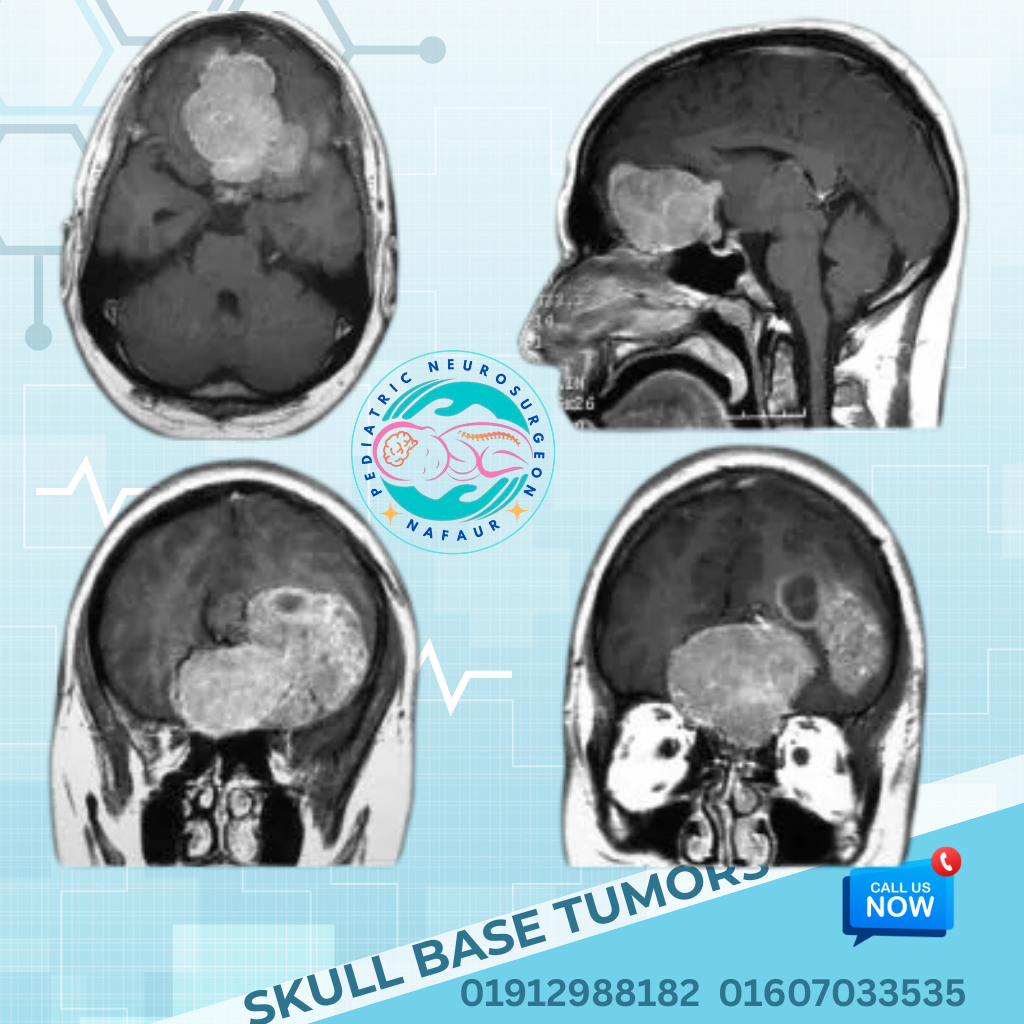
Skull Base Tumors
Skull base tumors are abnormal growths located at the base of the skull, where the brain meets the facial bones, sinuses, and spine. In children, skull base tumors are rare but can be extremely complex due to their deep location near critical structures such as cranial nerves, major blood vessels, the brainstem, and pituitary gland.
Pediatric skull base tumors are diverse in type, and their treatment often requires specialized surgical expertise, advanced neuroimaging, and a multidisciplinary approach. In Bangladesh, most such cases are referred late due to limited access to pediatric neurosurgical care. With the increasing availability of advanced facilities at NINS and Bangladesh Paediatric Neurocare Centre, outcomes for these tumors have improved significantly under the expert care of Dr. Md. Nafaur Rahman.
 Types of Pediatric Skull Base Tumors
Skull base tumors in children may be congenital, benign, or malignant, and can arise from various tissues such as bone, nerve, glandular, or vascular elements.
Common Pediatric Skull Base Tumors:
Chordomas – Rare, slow-growing bone tumors typically at the clivus
Chondrosarcomas – Malignant tumors arising from cartilage
Craniopharyngiomas – Tumors arising near the sellar/suprasellar region
Pituitary Adenomas (in adolescents) – Can affect hormonal regulation
Nasopharyngeal Angiofibromas – Highly vascular tumors often seen in adolescent males
Schwannomas – Arising from cranial nerves (e.g., vestibular or trigeminal nerves)
Meningiomas – Rare in children but possible in congenital forms
Dermoid and Epidermoid Cysts – Benign but may cause compression
Esthesioneuroblastomas and Sarcomas – Rare malignant tumors of nasal/skull base origin
Each of these tumors requires a tailored surgical and medical plan depending on the location, type, and impact on surrounding brain structures.
Types of Pediatric Skull Base Tumors
Skull base tumors in children may be congenital, benign, or malignant, and can arise from various tissues such as bone, nerve, glandular, or vascular elements.
Common Pediatric Skull Base Tumors:
Chordomas – Rare, slow-growing bone tumors typically at the clivus
Chondrosarcomas – Malignant tumors arising from cartilage
Craniopharyngiomas – Tumors arising near the sellar/suprasellar region
Pituitary Adenomas (in adolescents) – Can affect hormonal regulation
Nasopharyngeal Angiofibromas – Highly vascular tumors often seen in adolescent males
Schwannomas – Arising from cranial nerves (e.g., vestibular or trigeminal nerves)
Meningiomas – Rare in children but possible in congenital forms
Dermoid and Epidermoid Cysts – Benign but may cause compression
Esthesioneuroblastomas and Sarcomas – Rare malignant tumors of nasal/skull base origin
Each of these tumors requires a tailored surgical and medical plan depending on the location, type, and impact on surrounding brain structures.
 Symptoms of Skull Base Tumors in Children
Symptoms vary depending on the exact location and size of the tumor, but many skull base tumors may cause:
Vision problems (blurry vision, double vision, vision loss)
Hearing loss or ringing in the ears (tinnitus)
Facial numbness or weakness
Headache and vomiting (from raised intracranial pressure)
Hormonal imbalances (if the tumor affects the pituitary gland)
Nasal obstruction or frequent nosebleeds (especially in nasopharyngeal tumors)
Seizures or behavioral changes
Imbalance or gait problems (if the brainstem is involved)
In Bangladesh, these symptoms are often misdiagnosed as sinusitis, ENT problems, or behavioral disorders, delaying proper intervention.
Symptoms of Skull Base Tumors in Children
Symptoms vary depending on the exact location and size of the tumor, but many skull base tumors may cause:
Vision problems (blurry vision, double vision, vision loss)
Hearing loss or ringing in the ears (tinnitus)
Facial numbness or weakness
Headache and vomiting (from raised intracranial pressure)
Hormonal imbalances (if the tumor affects the pituitary gland)
Nasal obstruction or frequent nosebleeds (especially in nasopharyngeal tumors)
Seizures or behavioral changes
Imbalance or gait problems (if the brainstem is involved)
In Bangladesh, these symptoms are often misdiagnosed as sinusitis, ENT problems, or behavioral disorders, delaying proper intervention.
 Diagnosis & Evaluation
A complete diagnostic work-up is crucial to determine the nature, extent, and operability of the skull base tumor. Dr. Nafaur Rahman ensures a step-by-step, accurate assessment:
MRI Brain and Skull Base with Contrast – Best for assessing tumor anatomy and relation to neural structures
CT Scan with 3D Reconstruction – For bone involvement
Angiography or MR Angio (MRA) – For vascular tumors
Hormonal blood tests – Especially in sellar/suprasellar lesions
Biopsy or intraoperative frozen section – In selected cases for definitive diagnosis
Ophthalmologic, ENT, and endocrinology evaluations – As part of multidisciplinary planning
These evaluations are conducted at NINS and BP Neurocare Centre, under one coordinated system to reduce delays and optimize planning.
Diagnosis & Evaluation
A complete diagnostic work-up is crucial to determine the nature, extent, and operability of the skull base tumor. Dr. Nafaur Rahman ensures a step-by-step, accurate assessment:
MRI Brain and Skull Base with Contrast – Best for assessing tumor anatomy and relation to neural structures
CT Scan with 3D Reconstruction – For bone involvement
Angiography or MR Angio (MRA) – For vascular tumors
Hormonal blood tests – Especially in sellar/suprasellar lesions
Biopsy or intraoperative frozen section – In selected cases for definitive diagnosis
Ophthalmologic, ENT, and endocrinology evaluations – As part of multidisciplinary planning
These evaluations are conducted at NINS and BP Neurocare Centre, under one coordinated system to reduce delays and optimize planning.
 Surgical Management of Skull Base Tumors
Surgical resection is the cornerstone of treatment for many pediatric skull base tumors. Dr. Md. Nafaur Rahman is trained in advanced skull base and minimally invasive techniques, ensuring safe tumor removal with the best functional outcomes.
Surgical Approaches:
Endoscopic Endonasal Skull Base Surgery – Minimally invasive access for midline tumors such as craniopharyngiomas and pituitary adenomas
Open Skull Base Approaches – Including transcranial, subtemporal, infratemporal, and retrosigmoid routes
Combined Neurosurgical & ENT/Maxillofacial Surgery – For extensive tumors
Microsurgical Dissection – To preserve vital nerves and vessels
Intraoperative Navigation & Monitoring – To ensure precision and safety
Cyst drainage or shunt placement – In cases with hydrocephalus
"Operating on pediatric skull base tumors demands not just surgical skill but also anatomical finesse. In Bangladesh, we now have the tools and experience to treat these conditions safely and successfully."
— Dr. Md. Nafaur Rahman
Surgical Management of Skull Base Tumors
Surgical resection is the cornerstone of treatment for many pediatric skull base tumors. Dr. Md. Nafaur Rahman is trained in advanced skull base and minimally invasive techniques, ensuring safe tumor removal with the best functional outcomes.
Surgical Approaches:
Endoscopic Endonasal Skull Base Surgery – Minimally invasive access for midline tumors such as craniopharyngiomas and pituitary adenomas
Open Skull Base Approaches – Including transcranial, subtemporal, infratemporal, and retrosigmoid routes
Combined Neurosurgical & ENT/Maxillofacial Surgery – For extensive tumors
Microsurgical Dissection – To preserve vital nerves and vessels
Intraoperative Navigation & Monitoring – To ensure precision and safety
Cyst drainage or shunt placement – In cases with hydrocephalus
"Operating on pediatric skull base tumors demands not just surgical skill but also anatomical finesse. In Bangladesh, we now have the tools and experience to treat these conditions safely and successfully."
— Dr. Md. Nafaur Rahman
 Multimodal Therapy & Rehabilitation
For certain tumors (e.g., chordomas, sarcomas, or malignant schwannomas), additional therapies may be needed:
Radiotherapy – Stereotactic or proton beam therapy for deep-seated or residual tumors
Chemotherapy – For malignant or unresectable tumors
Hormone Replacement Therapy – Post-surgical pituitary dysfunction
Rehabilitation Services – Physiotherapy, speech therapy, and psychological support
Multimodal Therapy & Rehabilitation
For certain tumors (e.g., chordomas, sarcomas, or malignant schwannomas), additional therapies may be needed:
Radiotherapy – Stereotactic or proton beam therapy for deep-seated or residual tumors
Chemotherapy – For malignant or unresectable tumors
Hormone Replacement Therapy – Post-surgical pituitary dysfunction
Rehabilitation Services – Physiotherapy, speech therapy, and psychological support
 Pediatric Skull Base Tumors in Bangladesh – The Road Ahead
In Bangladesh, pediatric skull base tumors are often underreported due to lack of awareness and diagnostic facilities. Challenges include:
Misdiagnosis or delayed diagnosis
Limited specialized centers outside Dhaka
Financial burden on families
Shortage of pediatric neurosurgical expertise
Dr. Nafaur Rahman is working to address these gaps by providing affordable, specialized, and accessible skull base surgery for children throughout Bangladesh.
Pediatric Skull Base Tumors in Bangladesh – The Road Ahead
In Bangladesh, pediatric skull base tumors are often underreported due to lack of awareness and diagnostic facilities. Challenges include:
Misdiagnosis or delayed diagnosis
Limited specialized centers outside Dhaka
Financial burden on families
Shortage of pediatric neurosurgical expertise
Dr. Nafaur Rahman is working to address these gaps by providing affordable, specialized, and accessible skull base surgery for children throughout Bangladesh.
 Why Choose Dr. Md. Nafaur Rahman?
Why Choose Dr. Md. Nafaur Rahman?
 Pioneer in complex pediatric skull base surgery in Bangladesh
Pioneer in complex pediatric skull base surgery in Bangladesh
 Access to advanced intraoperative tools and endoscopy systems
Access to advanced intraoperative tools and endoscopy systems
 Patient-centered approach with family education and follow-up
Patient-centered approach with family education and follow-up
 Deep commitment to improving pediatric neurosurgical outcomes in Bangladesh
Deep commitment to improving pediatric neurosurgical outcomes in Bangladesh
 Excellent outcomes with multidisciplinary support
Excellent outcomes with multidisciplinary support
 Contact for Pediatric Skull Base Tumor Consultation
Dr. Md. Nafaur Rahman
Assistant Professor, Pediatric Neurosurgery, NINS
Chief Consultant, Bangladesh Paediatric Neurocare Centre
Contact for Pediatric Skull Base Tumor Consultation
Dr. Md. Nafaur Rahman
Assistant Professor, Pediatric Neurosurgery, NINS
Chief Consultant, Bangladesh Paediatric Neurocare Centre
 For Serial/Appointment: 01912988182 | 01607033535
For Serial/Appointment: 01912988182 | 01607033535
 Website: www.neurosurgeonnafaur.com
Website: www.neurosurgeonnafaur.com