Schizencephaly
Schizencephaly
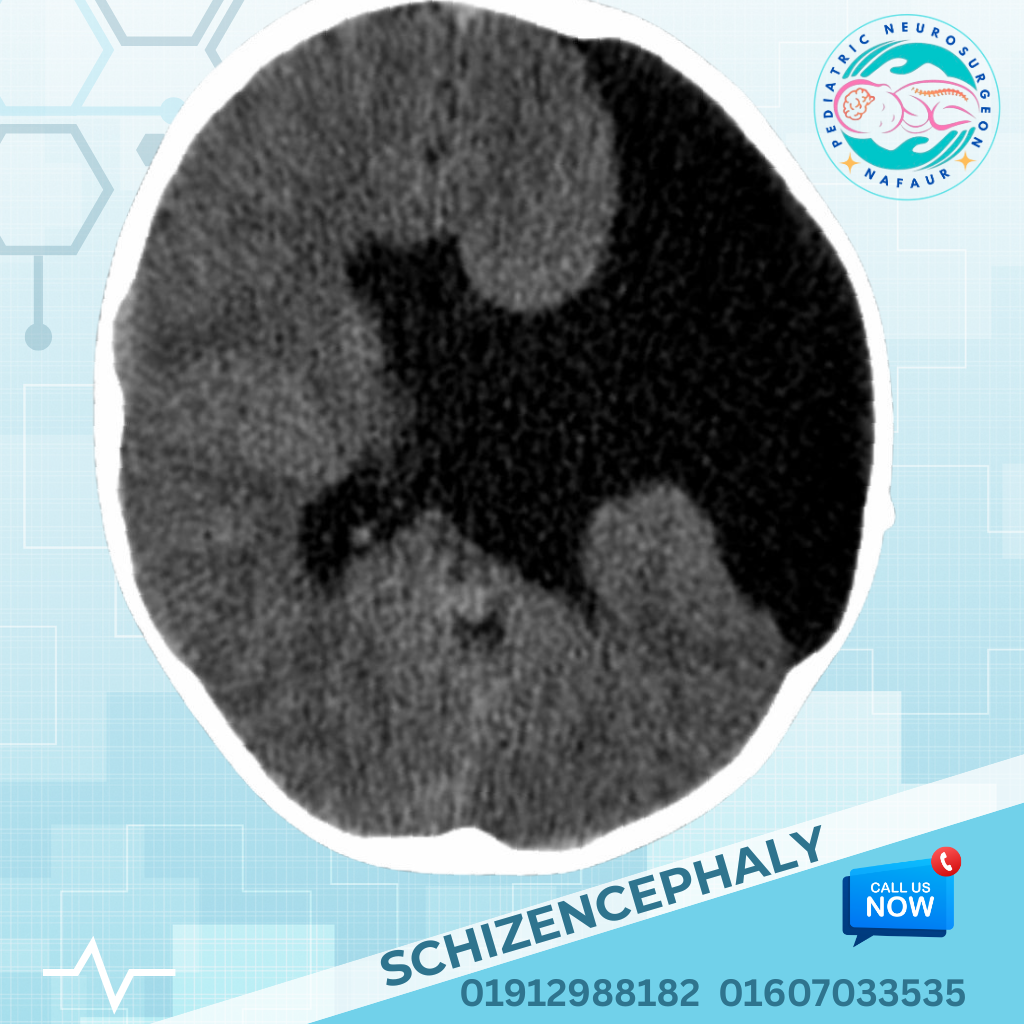
Schizencephaly is a rare and serious congenital brain malformation characterized by abnormal clefts or slits in the cerebral hemispheres that extend from the brain's surface (pial surface) to the lateral ventricles. These clefts are lined with gray matter, indicating abnormal migration of neurons during early fetal brain development (usually before the 8th week of gestation). Schizencephaly affects brain function depending on the size, location, and type of cleft, often leading to seizures, developmental delay, muscle weakness, and intellectual disabilities. Early diagnosis and neurosurgical evaluation are essential to manage complications such as hydrocephalus, intractable epilepsy, and motor dysfunction. 🌍 Schizencephaly in Bangladesh: A Growing Concern In Bangladesh, due to limited prenatal neuroimaging and awareness of congenital brain malformations, schizencephaly is often diagnosed late—after the child begins showing symptoms like seizures, poor motor skills, or delayed development. The disorder may be mistaken for cerebral palsy or other neurological conditions. With rising access to MRI brain scans, early neurodevelopmental screening, and expert pediatric neurosurgical services at institutions like NINS and Bangladesh Paediatric Neurocare Centre, children with schizencephaly in Bangladesh are now receiving more timely and effective care. 🧠 Types of Schizencephaly Schizencephaly is classified into two main types based on the structure of the cleft: Type I (Closed-lip schizencephaly): The cleft walls are in contact or fused Type II (Open-lip schizencephaly): The cleft walls are separated, often filled with cerebrospinal fluid (CSF) It may be unilateral (affecting one hemisphere) or bilateral (both hemispheres), with bilateral open-lip forms being more severe and associated with extensive neurological impairment. ⚠️ Causes and Risk Factors Defective neuronal migration during the first trimester Intrauterine infections (e.g., cytomegalovirus - CMV) Prenatal vascular injuries or stroke Teratogen exposure (alcohol, drugs, or toxins during pregnancy) Genetic mutations (EMX2 gene in rare familial cases) Often sporadic with no family history 🧒 Symptoms and Clinical Presentation The severity of symptoms depends on the type, size, and location of the cleft. Common symptoms include: Seizures – often focal and drug-resistant Developmental delay – especially in gross motor and language skills Spasticity or hypotonia – typically hemiparesis or quadriparesis Microcephaly – in some severe cases Hydrocephalus – especially in open-lip schizencephaly Learning and intellectual disability Visual disturbances – such as strabismus or cortical blindness Feeding and swallowing difficulties (in severe bilateral cases) 🔍 Diagnosis and Imaging 1. MRI Brain (Gold Standard) Reveals clefts extending from the brain surface to ventricles Gray matter lining of clefts confirms diagnosis Helps differentiate from porencephaly or other cystic lesions 2. CT Scan Useful where MRI is unavailable, though less sensitive Can detect associated hydrocephalus or calcifications 3. EEG Essential for identifying seizure focus and type Helps in planning epilepsy surgery when needed 4. Genetic Testing In selected cases with family history or syndromic features 🛠️ Treatment and Neurosurgical Management There is no cure for schizencephaly, but many of its complications can be effectively managed with a multidisciplinary approach, including neurosurgery, neurology, physiotherapy, and special education. 1. Seizure Management Anti-epileptic drugs (AEDs) are first-line In cases of drug-resistant epilepsy, surgical options may include: Focal cortical resection Lobectomy Corpus callosotomy (for drop attacks or generalized seizures) Vagus nerve stimulation (VNS) 2. Hydrocephalus Treatment Common in open-lip types due to CSF obstruction Requires VP shunt or Endoscopic Third Ventriculostomy (ETV) 3. Spasticity and Motor Dysfunction Managed with physiotherapy, botulinum toxin injections, or selective dorsal rhizotomy (SDR) in selected cases 4. Neurorehabilitation Regular physical therapy, occupational therapy, and speech therapy Use of assistive devices for mobility and communication Inclusion in special education programs 🔄 Prognosis Unilateral closed-lip schizencephaly: Often associated with milder symptoms; some children may attend mainstream school with therapy Bilateral open-lip schizencephaly: Severe neurological disability, often with significant developmental delays and mobility challenges Early intervention is key to improving outcomes Regular follow-up with pediatric neurologists and neurosurgeons is essential 👨⚕️ Why Trust Dr. Md. Nafaur Rahman? One of Bangladesh’s most experienced pediatric neurosurgeons, with specific expertise in congenital brain malformations Provides comprehensive diagnosis, surgical treatment, and long-term follow-up for schizencephaly Offers integrated care through the Bangladesh Paediatric Neurocare Centre, ensuring access to therapy, imaging, and neurology in one setting Performs VP shunts, epilepsy surgeries, and multidisciplinary care coordination under one roof at NINS 📞 Schedule an Expert Evaluation Today Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, NINS Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Appointment: 01912988182 | 01607033535 🌐 Visit: www.neurosurgeonnafaur.com