Diffuse Axonal Injury
Diffuse Axonal Injury
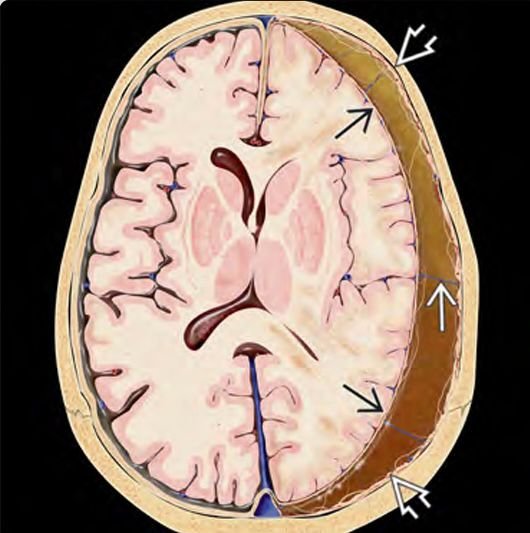
Diffuse Axonal Injury (DAI) is one of the most severe and life-threatening forms of traumatic brain injury (TBI) in children. It involves widespread damage to the brain's white matter tracts due to rapid acceleration-deceleration forces, commonly seen in road traffic accidents, falls from height, or non-accidental trauma such as Shaken Baby Syndrome. In Bangladesh, pediatric DAI often remains underdiagnosed due to limited awareness and inadequate access to specialized neuroimaging and critical care. Dr. Md. Nafaur Rahman, a leading pediatric neurosurgeon in Bangladesh, specializes in the diagnosis, neurocritical management, and rehabilitation of pediatric patients suffering from diffuse axonal injury. Early identification and appropriate ICU-based treatment can significantly improve outcomes for affected children. What is Pediatric Diffuse Axonal Injury? Diffuse Axonal Injury (DAI) occurs when the brain undergoes sudden rotational or shearing forces, causing microscopic tears in the axons (the long nerve fibers responsible for brain communication). Unlike focal injuries, DAI affects multiple brain areas simultaneously, especially: Corpus callosum Brainstem Cerebral white matter Midbrain and thalamus These injuries disrupt normal brain signaling and often result in prolonged coma, vegetative states, or severe neurocognitive deficits in survivors. Common Causes in the Bangladesh Context High-speed road traffic accidents involving motorcycles, rickshaws, or buses Falls from rooftops, trees, or staircases (especially in rural areas) Shaken Baby Syndrome or abusive head trauma in infants Sports injuries or playground accidents Birth-related trauma in severe delivery complications Symptoms and Clinical Presentation The hallmark of DAI is loss of consciousness at the time of injury and prolonged coma not explained by bleeding or swelling. Other signs include: Unresponsiveness or Glasgow Coma Score < 8 Decerebrate or decorticate posturing Seizures Breathing irregularities Abnormal pupil responses Autonomic instability (heart rate, temperature fluctuations) DAI is often suspected clinically when a child has a severe TBI with minimal visible injury on CT scan. Diagnosis of Pediatric DAI in Bangladesh Imaging CT Scan (initial): May be normal or show small punctate hemorrhages in severe cases MRI Brain (gold standard): Particularly Diffusion Tensor Imaging (DTI) or SWI (Susceptibility Weighted Imaging) can identify axonal shearing EEG: Used to evaluate coma and detect non-convulsive seizures Evoked potentials: For prognosis in prolonged unconsciousness Due to limited access to MRI in rural Bangladesh, many cases remain undiagnosed or misclassified as mild TBI. Management Approach by Dr. Md. Nafaur Rahman DAI requires a neurocritical care-centered approach rather than immediate surgery. Neurocritical Management ICU monitoring with mechanical ventilation Intracranial pressure (ICP) monitoring Head elevation and sedation to prevent brain swelling Anticonvulsants for seizure prevention Nutritional support and fluid balance Neuroprotective agents under clinical protocols Temperature control to reduce metabolic demand on the brain Neurosurgical Support Although DAI itself doesn’t usually require surgery, associated complications may include: Hematomas requiring evacuation CSF diversion (VP Shunt or EVD) for hydrocephalus Craniectomy in refractory intracranial hypertension Rehabilitation and Long-Term Outcome Many children with DAI who survive the acute phase require long-term neuro-rehabilitation, including: Physiotherapy and occupational therapy Speech and language therapy Psychological and behavioral counseling Special education planning With continued follow-up at the Bangladesh Paediatric Neurocare Centre, significant functional recovery is possible, especially in mild to moderate cases. Prognosis in Pediatric DAI Prognosis depends on: Severity of initial injury Duration of coma Response to critical care and rehabilitation Availability of support systems Mild DAI can recover with minimal deficits, while severe DAI may lead to persistent vegetative state, spasticity, epilepsy, or neurocognitive dysfunction. Challenges in Bangladesh Limited awareness among general physicians and emergency doctors Shortage of pediatric ICU beds in district hospitals Delay in MRI diagnostics Insufficient rehabilitation centers for long-term therapy Social stigma and financial burden on families Dr. Nafaur Rahman actively works to bridge the gap in specialized pediatric neurotrauma care through outreach, education, and modern treatment facilities. Why Choose Dr. Md. Nafaur Rahman? Extensive experience in pediatric brain trauma and coma management Advanced neuroimaging interpretation skills in children Integrated critical care and neuro-rehabilitation protocols Works with a team of pediatric intensivists, therapists, and child psychologists Offers both inpatient and outpatient long-term follow-up care Contact for Consultation Dr. Md. Nafaur Rahman Assistant Professor, Department of Pediatric Neurosurgery, NINS Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial and Emergency Call: 📱 +8801912988182 | +8801607033535 🌐 Website: www.neurosurgeonnafaur.com
YouTube Videos and Patient Reviews on Diffuse Axonal Injury