Intracranial Hematomas
Intracranial Hematomas
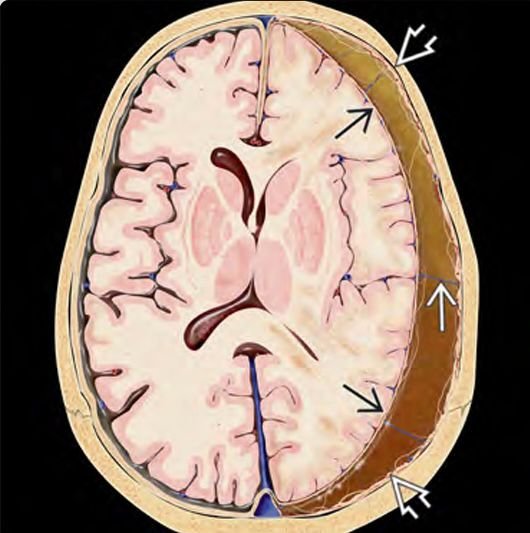
Intracranial hematomas in children are critical neurosurgical conditions characterized by the accumulation of blood within the cranial cavity, either inside the brain tissue or in spaces surrounding the brain. These hematomas often arise due to head trauma but may also be caused by vascular abnormalities, bleeding disorders, or spontaneous hemorrhage. In Bangladesh, pediatric intracranial hematomas represent a significant health challenge, especially with increasing rates of road traffic accidents, falls, and other injuries in children. Early diagnosis and prompt neurosurgical intervention are essential to reduce morbidity and mortality and to ensure optimal neurodevelopmental outcomes. Types of Pediatric Intracranial Hematomas There are several types of intracranial hematomas in pediatric patients, each with distinct clinical features, locations, and treatment approaches: Epidural Hematoma (EDH): Blood accumulation between the skull and the dura mater. Often caused by skull fractures with arterial bleeding, especially the middle meningeal artery. Subdural Hematoma (SDH): Blood collects between the dura mater and arachnoid membrane. Common in infants and young children due to falls or non-accidental trauma (shaken baby syndrome). Intracerebral Hematoma (ICH): Bleeding within the brain tissue itself, usually resulting from severe trauma or vascular lesions. Subarachnoid Hemorrhage (SAH): Bleeding into the subarachnoid space, frequently caused by trauma or vascular anomalies. Intraventricular Hemorrhage (IVH): Bleeding inside the brain’s ventricular system, mainly seen in premature neonates but can occur in older children. Causes and Risk Factors in Bangladesh Traumatic Brain Injury (TBI): The leading cause, primarily due to road traffic accidents, falls from height, and domestic accidents. Non-Accidental Injury: Child abuse resulting in subdural hematomas and other intracranial bleeding. Vascular Malformations: Including aneurysms and arteriovenous malformations that predispose to spontaneous bleeding. Bleeding Disorders: Such as hemophilia and thrombocytopenia, prevalent in some pediatric populations. Infections and Tumors: Rare causes involving vascular invasion or coagulopathy. Clinical Presentation Symptoms vary by hematoma type and severity but generally include: Severe headache and vomiting Altered consciousness or coma Seizures or convulsions Focal neurological deficits such as weakness, paralysis, or sensory loss Scalp swelling or bruising following trauma Irritability or lethargy in infants Early recognition of symptoms is critical to prompt medical evaluation and treatment. Diagnosis Neuroimaging: CT Scan: The gold standard for rapid detection of intracranial hematomas, determining size, location, and mass effect. MRI: Provides detailed brain tissue evaluation and is useful for assessing underlying causes or complications. Neurological Examination: Including pediatric Glasgow Coma Scale and focal deficit assessment. Laboratory Tests: To identify coagulopathies or infections. Treatment by Dr. Md. Nafaur Rahman Medical Management Close monitoring in Pediatric Intensive Care Units (PICU) Control of intracranial pressure with medications (mannitol, hypertonic saline) Seizure control with anticonvulsants Correction of underlying bleeding disorders Supportive care including oxygenation, hydration, and nutritional support Surgical Intervention Indicated for large hematomas causing brain compression or neurological deterioration Procedures include craniotomy, hematoma evacuation, and decompressive surgery tailored to pediatric anatomy Postoperative care focuses on neurocritical monitoring and rehabilitation Prognosis and Follow-up Outcomes depend on early intervention, hematoma size, location, and patient’s overall health. With prompt treatment, many children achieve good recovery; however, severe cases may result in long-term neurological deficits, developmental delays, or epilepsy. Regular follow-up includes: Neurodevelopmental assessments Physical, occupational, and speech therapy Imaging studies to monitor for recurrence or complications Pediatric Neurosurgical Services in Bangladesh Dr. Md. Nafaur Rahman leads expert pediatric neurosurgical care at the National Institute of Neurosciences & Hospital (NINS) and Bangladesh Paediatric Neurocare Centre. His comprehensive approach integrates: Advanced imaging and surgical techniques Multidisciplinary care teams Family education and counseling Emphasis on early diagnosis, intervention, and rehabilitation Contact Information for Pediatric Neurosurgical Care 📌 Dr. Md. Nafaur Rahman Assistant Professor, Department of Pediatric Neurosurgery, NINS Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Appointment & Emergency: 📱 +8801912988182 | +8801607033535 🌐 www.neurosurgeonnafaur.com
YouTube Videos and Patient Reviews on Intracranial Hematomas