Skull metastatic tumors
Skull metastatic tumors
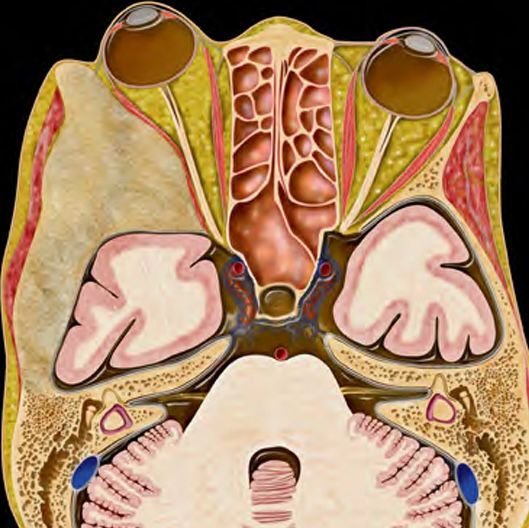
Skull metastatic tumors in children are rare but clinically significant conditions where cancer from another part of the body spreads to the bones of the skull. These tumors may present as a painful or painless lump, neurological symptoms, or cranial nerve dysfunction depending on the location. While skull metastases are more common in adults, pediatric cases are increasingly being recognized, particularly in patients with known primary malignancies such as neuroblastoma, leukemia, Ewing sarcoma, or rhabdomyosarcoma. In Bangladesh, due to low awareness, lack of early neuroimaging, and misdiagnosis as scalp abscess or infection, skull metastases in children are often detected late. Dr. Md. Nafaur Rahman, one of Bangladesh's foremost pediatric neurosurgeons, offers specialized expertise in identifying, evaluating, and surgically managing pediatric skull metastases in coordination with pediatric oncology teams. What Are Skull Metastatic Tumors? A skull metastatic tumor refers to the spread of cancer cells to the cranial bones from a primary tumor elsewhere in the body. These secondary tumors can invade: The calvarial bones (frontal, parietal, occipital) The skull base (temporal, sphenoid, occipital condyles) The diploic space, potentially extending into the scalp or dura Common Pediatric Cancers That Metastasize to Skull Neuroblastoma – most common solid cancer in young children with bony metastases Ewing Sarcoma – aggressive bone tumor with skull involvement Leukemia – infiltration into skull with subgaleal or subdural spread Rhabdomyosarcoma – may extend into cranial bones Lymphoma – cranial bone involvement as part of systemic disease Medulloblastoma and other brain tumors – rarely spread to skull via cerebrospinal fluid seeding Clinical Presentation Children with skull metastases may present with: Lump or swelling on the head (commonly firm and fixed) Localized pain or tenderness over the area Scalp discoloration or vascular changes Headache, nausea, vomiting if intracranial pressure rises Cranial nerve deficits if skull base is involved Neurological weakness or seizures if the brain is compressed Systemic signs of malignancy: fever, weight loss, fatigue, pallor In rural Bangladesh, these symptoms are often misinterpreted as infection, trauma-related swelling, or benign cysts, delaying the correct diagnosis. Importance of Early Detection in Bangladesh Delayed diagnosis can lead to skull bone destruction, intracranial spread, and poor prognosis Misdiagnosis leads to incorrect antibiotic use or drainage attempts Awareness and access to imaging are limited outside Dhaka and major centers Diagnostic Strategy Dr. Md. Nafaur Rahman follows a comprehensive, multi-step diagnostic protocol: 1. Detailed Clinical History Known history of cancer or suspicious systemic illness Examination for neurological deficits or cranial nerve involvement 2. Imaging Studies Skull X-ray: Shows lytic lesions or bony destruction MRI with contrast: Gold standard for identifying soft tissue extension and brain involvement CT Scan: Assesses bone erosion and skull base involvement PET scan / bone scan: For staging and identifying systemic spread 3. Biopsy Open or needle biopsy confirms the diagnosis Pathology reveals type of tumor, important for treatment planning Treatment Approach A. Multidisciplinary Collaboration Management involves a team including pediatric neurosurgeon, oncologist, radiotherapist, and pathologist B. Surgical Management Dr. Nafaur Rahman performs neurosurgical intervention for: Diagnostic biopsy Tumor excision when accessible and necessary Decompression of the brain or cranial nerves Cranial reconstruction (cranioplasty) if there’s bone loss Minimally invasive or open approach based on tumor location C. Chemotherapy & Radiotherapy Primary tumor management continues under oncologists Chemotherapy is often effective in shrinking metastatic lesions Radiotherapy is used in select cases, especially with spinal or skull base involvement Prognosis Prognosis depends on type and stage of primary tumor Local control of skull lesions improves quality of life and neurological function Early neurosurgical involvement leads to better outcomes Surveillance MRI is essential for follow-up Challenges in Bangladesh Low awareness among general physicians Misdiagnosis as trauma or infection Late referral to specialized neurosurgical centers Limited access to pediatric MRI or biopsy facilities outside major cities Financial and emotional burden on families Why Choose Dr. Md. Nafaur Rahman? Expertise in pediatric cranial tumor and skull lesion surgery Performs safe, precise skull tumor resections with attention to cosmetic outcomes Collaborates with leading pediatric oncology units in Bangladesh Offers services at both National Institute of Neurosciences & Hospital (NINS) and Bangladesh Paediatric Neurocare Centre Committed to affordable, compassionate, and child-friendly care Contact for Consultation Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Appointment/Serial: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com