Rhabdomyosarcoma
Rhabdomyosarcoma
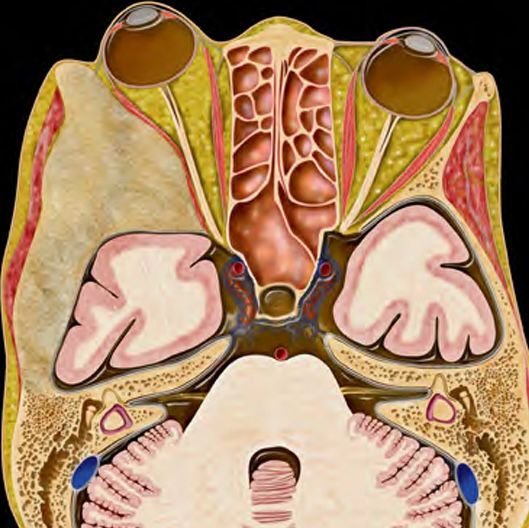
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma in children, arising from immature skeletal muscle cells. Though it can develop anywhere in the body, in pediatric neurosurgical practice, it may present in the head and neck region, cranial base, orbit, or even within the spine or skull vault. It is a high-grade malignant tumor requiring prompt diagnosis and a multidisciplinary treatment approach involving surgery, chemotherapy, and radiotherapy. In Bangladesh, early recognition and expert management of rhabdomyosarcoma in children remain a challenge. Many cases present late or are initially misdiagnosed. Dr. Md. Nafaur Rahman, one of the country's leading pediatric neurosurgeons, specializes in the neurosurgical management of head, neck, skull base, and spinal rhabdomyosarcomas in children, offering comprehensive care through both NINS and Bangladesh Paediatric Neurocare Centre. What is Rhabdomyosarcoma? Rhabdomyosarcoma is a malignant tumor that arises from mesenchymal cells committed to skeletal muscle lineage. It accounts for nearly 5% of all pediatric cancers and over 50% of soft tissue sarcomas in children. Though most commonly found in areas with skeletal muscle, it can also arise in the brain coverings, nasopharynx, orbit, and spinal regions, which require specialized neurosurgical attention. Common Sites in Pediatric Patients Head and Neck Region (35–40%) – orbit, nasopharynx, skull base Genitourinary tract Extremities Spine and paraspinal region Intracranial or skull-based tumors Types of Rhabdomyosarcoma Embryonal RMS (most common in young children) – relatively favorable prognosis Alveolar RMS – more aggressive and common in older children Pleomorphic RMS – rare, typically in adolescents Spindle/sclerosing RMS – rare variants with variable behavior Causes and Risk Factors Unknown in most cases Some association with Li-Fraumeni syndrome, Neurofibromatosis type 1, and Beckwith-Wiedemann syndrome No clear environmental or lifestyle risk factors Clinical Presentation in Neurosurgical Context When RMS affects the head, neck, skull base, or spine, symptoms can include: Head & Neck RMS: Painless or painful swelling Nasal obstruction, bleeding, or discharge Facial asymmetry Proptosis (bulging eye) in orbital RMS Vision changes, cranial nerve palsy, or headache Spinal/Paraspinal RMS: Back pain, limb weakness Sensory changes or paralysis Bladder or bowel incontinence These symptoms are often mistaken for benign conditions like infections, cysts, or sinusitis in Bangladesh, causing treatment delay. Diagnosis Dr. Nafaur Rahman follows a systematic and evidence-based protocol for early diagnosis. 1. Clinical Examination Complete pediatric neurological and craniofacial assessment Evaluation of lymph nodes and associated syndromic features 2. Imaging Studies MRI with contrast – preferred for soft tissue evaluation, extent, and surgical planning CT Scan – useful for bony involvement and skull base anatomy PET-CT or bone scan – for staging and detecting metastasis 3. Biopsy and Histopathology Image-guided core needle biopsy or open surgical biopsy Immunohistochemistry: Desmin, myogenin, MyoD1 positivity confirms RMS Genetic testing: PAX3/7-FOXO1 fusion for alveolar subtype Treatment Approach Treatment of rhabdomyosarcoma involves a multidisciplinary, multimodal strategy: A. Surgical Management Surgery is vital for: Biopsy for diagnosis Complete or partial excision of the tumor when feasible Neurosurgical decompression if the brain, spinal cord, or optic structures are compressed Craniofacial or skull base reconstruction when needed Dr. Nafaur Rahman uses minimally invasive, microscope-assisted, and neuronavigation-guided techniques to ensure maximal tumor resection with minimal functional or cosmetic impact. B. Chemotherapy Backbone of treatment for all RMS types Standard drugs: Vincristine, Actinomycin D, Cyclophosphamide (VAC regimen) Adjusted based on tumor risk stratification and subtype C. Radiotherapy Indicated in cases where complete resection isn’t possible Also used in metastatic or recurrent cases Delivered with precision techniques to reduce side effects in children Prognosis Embryonal RMS has up to 70–80% survival in localized disease Alveolar RMS and metastatic cases have poorer outcomes Prognosis depends on tumor site, size, spread, and surgical accessibility Challenges in Bangladesh Low awareness about childhood cancer Initial misdiagnosis as infection or benign swelling Inadequate referral to pediatric oncology or neurosurgery Delayed imaging due to cost or inaccessibility Social stigma and treatment abandonment in rural areas Why Dr. Md. Nafaur Rahman? Leading expert in neurosurgical oncology for children in Bangladesh Skilled in managing complex skull base, orbital, and spinal tumors Works with a multidisciplinary oncology team for comprehensive care Offers affordable treatment pathways through both government (NINS) and private (Bangladesh Paediatric Neurocare Centre) setups Compassionate, child-focused care with emphasis on function preservation and quality of life Contact for Serial & Consultation Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Appointment/Serial: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com