Neurofibroma
Neurofibroma
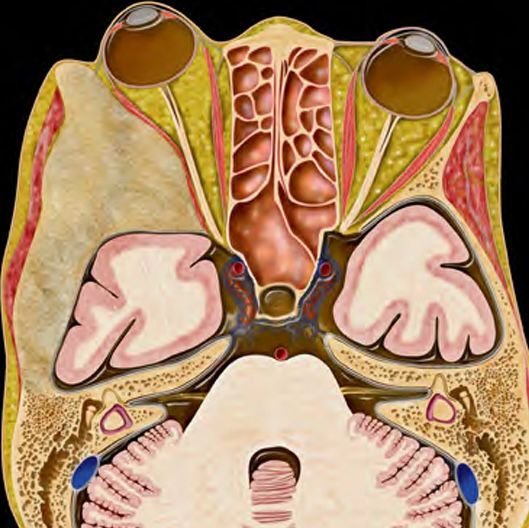
Scalp neurofibromas are benign nerve sheath tumors that develop from peripheral nerves under the scalp. Though most commonly associated with Neurofibromatosis Type 1 (NF1), isolated neurofibromas can also occur in children without any underlying genetic disorder. These lesions may present as painless lumps or nodules on the scalp and can progressively increase in size, leading to cosmetic disfigurement or, in rare cases, neurological symptoms due to involvement of deeper structures. In Bangladesh, where dermatologic scalp swellings in children are often under-investigated, Dr. Md. Nafaur Rahman, a leading pediatric neurosurgeon at the National Institute of Neurosciences & Hospital (NINS) and Bangladesh Paediatric Neurocare Centre, offers advanced diagnostic and surgical solutions to safely treat scalp neurofibromas in children. What is a Scalp Neurofibroma? A neurofibroma is a benign tumor composed of Schwann cells, fibroblasts, and nerve axons. When located on the scalp, it typically arises from small cutaneous or subcutaneous nerves in the scalp’s dermal or subdermal layers. In pediatric patients, neurofibromas may be: Solitary (localized) – not associated with any syndrome Plexiform – larger, irregular, and often linked to Neurofibromatosis Type 1 (NF1) Multiple – in the context of syndromic diagnosis Causes and Risk Factors Genetic mutation in the NF1 gene (for syndromic cases) Sporadic mutations for isolated, non-syndromic neurofibromas Family history of neurofibromatosis increases the risk Clinical Features in Children Scalp neurofibromas may present with: Painless, soft or firm lump on the scalp Slow but progressive growth over months or years Cosmetic concern, especially if visible on frontal or temporal regions Skin pigmentation or café-au-lait spots in NF1 patients Hair loss (alopecia) over the lesion In plexiform types: large, irregular, “bag of worms” feel Rarely: itching, tingling, or mild pain Very rarely: bony erosion or extension into the skull Importance of Early Detection in Bangladesh In rural and even urban areas of Bangladesh, parents often mistake these lesions for harmless cysts, lipomas, or abscesses. These are sometimes treated with antibiotics or even home remedies, delaying proper diagnosis. Delayed care can result in: Larger lesion size requiring more complex surgery Irreversible deformity or scarring Missed diagnosis of underlying Neurofibromatosis Type 1 (NF1) Diagnosis Dr. Md. Nafaur Rahman follows a multidisciplinary, child-focused diagnostic strategy for scalp neurofibromas. 1. Clinical Evaluation Detailed history, family history of NF1 Physical exam for associated neurocutaneous markers (e.g., café-au-lait spots, axillary freckling) 2. Imaging Studies Ultrasound (USG): Useful for superficial lesions MRI with contrast: Gold standard for evaluating extent, vascularity, and relationship with nearby structures CT scan: If bone involvement is suspected 3. Biopsy (if needed) Histopathology confirms diagnosis (presence of Schwann cells and fibrous stroma) Immunohistochemistry for S-100 protein helps differentiate from other tumors Treatment Approach Treatment is primarily surgical, especially for cosmetic correction, rapid growth, or risk of complications. Surgical Indications: Progressive enlargement Cosmetic disfigurement Suspicion of deeper involvement Associated with NF1 requiring tumor debulking Surgical Technique: Complete surgical excision under general anesthesia Minimal incision for better cosmetic outcome Preservation of surrounding nerves and tissues Cranioplasty if bony involvement or skull defect is present Postoperative histopathology to confirm nature of the lesion Postoperative Care & Outcome Most patients recover well with minimal scarring Rare recurrence, particularly in plexiform neurofibromas Follow-up every 6–12 months recommended for recurrence or new lesions For NF1 patients, lifelong neurological monitoring is advised Associated Conditions to Screen For If multiple neurofibromas or other signs of NF1 are seen, the following systems should be evaluated: Eyes: For optic gliomas Brain/spine MRI: For intracranial tumors or spinal neurofibromas Genetics: For definitive diagnosis of NF1 (if feasible) Challenges in Bangladesh Lack of pediatric neurosurgical awareness among general doctors Misdiagnosis as sebaceous cyst or lipoma Limited access to MRI in rural areas Cosmetic stigma for children in school settings Cultural barriers in seeking surgical treatment early Why Dr. Md. Nafaur Rahman? One of Bangladesh’s few pediatric neurosurgeons specializing in scalp and cranial soft-tissue tumors Expertise in minimally invasive surgical removal with cosmetic focus Uses high-resolution MRI and neuronavigation when needed Supports NF1 patients through a multidisciplinary care model Offers care both in government hospitals (NINS) and private clinics (Bangladesh Paediatric Neurocare Centre) Contact for Serial & Consultation Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 For Serial or Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com