Scalp Vascular Malformation
Scalp Vascular Malformation
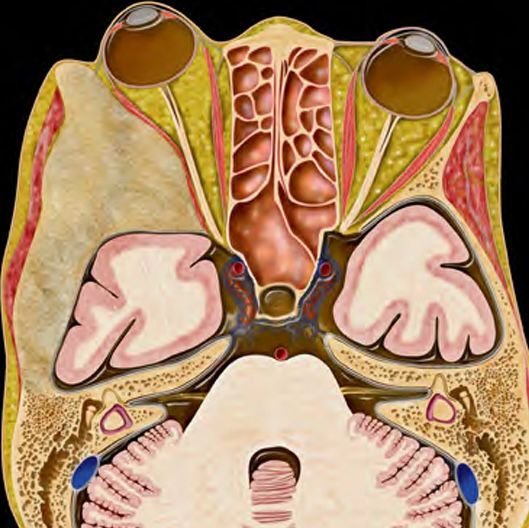
Scalp vascular malformations in children are rare but significant congenital anomalies involving abnormal blood vessels in the skin and soft tissues of the scalp. These malformations can involve arteries (arteriovenous malformations or AVMs), veins (venous malformations), capillaries, or lymphatic vessels. Some may remain small and asymptomatic, while others grow, pulsate, bleed, or cause cosmetic and functional issues. In Bangladesh, due to limited public awareness and diagnostic infrastructure, many children with scalp vascular malformations remain undiagnosed or misdiagnosed. Dr. Md. Nafaur Rahman, a leading pediatric neurosurgeon at NINS and Bangladesh Paediatric Neurocare Centre, provides expert evaluation and safe, effective surgical treatment for these rare but important conditions. Understanding Scalp Vascular Malformations Scalp vascular malformations are non-cancerous congenital lesions that result from abnormal development of blood vessels. Unlike hemangiomas (which are tumors), vascular malformations are structural abnormalities present at birth and grow proportionately with the child. Types of Vascular Malformations: Capillary Malformations (Port-Wine Stains) Flat, red or pink discoloration of the scalp Often cosmetic in nature Venous Malformations Blue, soft, compressible masses Increase in size with crying, straining, or head dependency May thrombose or cause pain Arteriovenous Malformations (AVMs) High-flow lesions with abnormal connection between arteries and veins May present with pulsation, bruit (vascular sound), warmth, and overlying skin changes Risk of bleeding or ulceration Lymphatic Malformations Rare in the scalp May present as fluid-filled, spongy masses Clinical Presentation Children may present with: Visible swelling or lump on the scalp Bluish or reddish discoloration of the skin Swelling that increases in size during crying or lying down Pulsation or bruit over the lesion (especially in AVMs) Bleeding or ulceration in advanced cases Cosmetic deformity, especially in frontal and temporal regions Rarely, signs of intracranial extension or increased intracranial pressure Diagnostic Evaluation Proper diagnosis is key to safe and successful treatment. Dr. Md. Nafaur Rahman recommends a stepwise approach: Clinical Examination Assessment of lesion color, pulsatility, consistency, tenderness, compressibility History of trauma, bleeding, or progression Imaging Studies Doppler Ultrasound: First-line, identifies flow dynamics (low vs. high flow) MRI & MR Angiography (MRA): To evaluate lesion extent and vascular anatomy CT Angiography: Useful for assessing bone involvement and vascular complexity Digital Subtraction Angiography (DSA): Gold standard for AVMs before surgery or embolization Treatment Options The goal is to achieve safe removal or reduction of the lesion, minimize recurrence, and address cosmetic concerns. 1. Observation Suitable for small, asymptomatic, non-progressive lesions Requires regular monitoring 2. Endovascular Embolization Minimally invasive technique for high-flow AVMs Involves injecting embolic agents to reduce blood flow Often done prior to surgery to reduce intraoperative bleeding 3. Surgical Excision Indicated for symptomatic or cosmetically disfiguring lesions Dr. Nafaur Rahman performs careful dissection using microsurgical techniques Use of neuronavigation, intraoperative ultrasound, and cosmetic reconstruction ensures best results Complete excision is critical to prevent recurrence 4. Combined Treatment For complex lesions, a multidisciplinary approach is adopted including interventional radiology, plastic surgery, and neurosurgery Postoperative Care and Prognosis Most children recover fully with excellent cosmetic outcomes Minimal scarring and recurrence when treated appropriately Postoperative care includes wound monitoring, follow-up imaging, and counseling Emotional and psychological support provided for both parents and child Special Considerations in Bangladesh Late diagnosis due to limited rural healthcare awareness Misdiagnosis as cysts, trauma, or birthmarks Limited availability of pediatric neurovascular imaging in peripheral hospitals High importance of early referral to specialized centers like NINS and Bangladesh Paediatric Neurocare Centre Why Choose Dr. Md. Nafaur Rahman? One of the few neurosurgeons in Bangladesh with subspecialty expertise in pediatric scalp vascular lesions Uses modern surgical tools and techniques for safe, bloodless, and cosmetic surgery Experienced in treating both simple and complex vascular malformations Trusted by parents across Bangladesh for honest, ethical, and skillful care Facilities for both diagnosis and treatment under one roof at NINS and Neurocare Contact for Appointment Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial & Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com