Dermoid and Epidermoid Cysts
Dermoid and Epidermoid Cysts
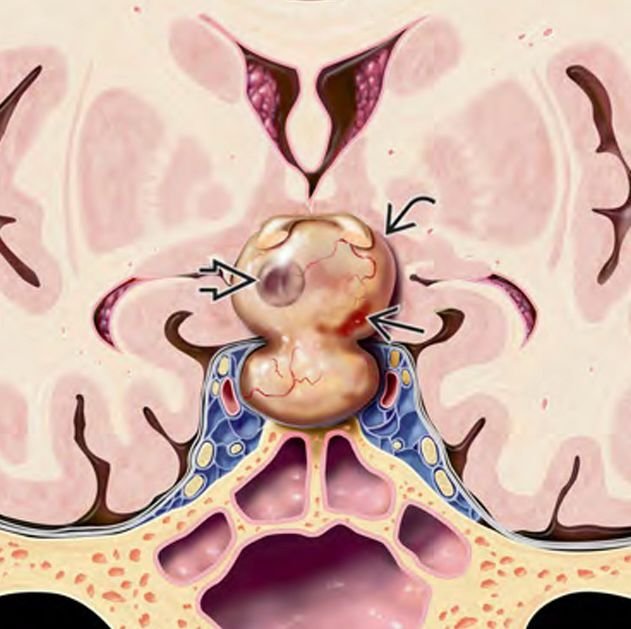
Dermoid and epidermoid cysts are rare congenital benign cystic lesions that occur due to developmental anomalies during embryogenesis. Located at the skull base, these cysts can grow slowly over years and cause symptoms by compressing adjacent neural structures. Though benign, their location near critical brainstem and cranial nerves requires expert diagnosis and surgical management, especially in pediatric patients. In Bangladesh, early detection and specialized treatment of these rare cysts are essential to prevent neurological deficits and improve long-term outcomes. Dr. Md. Nafaur Rahman offers advanced surgical expertise and compassionate care tailored to the unique needs of children with skull base cystic lesions. Epidemiology and Importance in Bangladesh Skull base dermoid and epidermoid cysts account for a small percentage of pediatric brain tumors but are important differential diagnoses in children presenting with neurological symptoms and skull base masses. Due to limited awareness and diagnostic facilities in many parts of Bangladesh, these lesions often remain undiagnosed or misdiagnosed, leading to delayed treatment. Children with unexplained headaches, cranial nerve dysfunction, or recurrent infections near the nasal or ear regions should be evaluated promptly at specialized centers such as NINS and the Bangladesh Paediatric Neurocare Centre for accurate diagnosis and management. Pathophysiology and Types Dermoid cysts contain ectodermal elements like hair follicles, sebaceous glands, and sometimes teeth, resulting from trapped skin tissue during neural tube closure. Epidermoid cysts are lined by stratified squamous epithelium and contain keratin debris, arising from inclusion of ectodermal cells during neural tube development. Both cysts are slow-growing and can cause mass effect symptoms as they enlarge. Common skull base locations include the cerebellopontine angle, parasellar region, clivus, and midline skull base. Clinical Presentation Symptoms vary based on cyst size and location but often include: Headaches – persistent and worsening Cranial nerve deficits such as facial weakness, hearing loss, or double vision Balance and coordination problems due to brainstem or cerebellar compression Recurrent meningitis or infections if cyst ruptures or leaks content Hydrocephalus in cases with obstructed cerebrospinal fluid flow Visible or palpable mass in rare superficial cases Children may present with subtle symptoms, requiring a high index of suspicion. Diagnostic Approach Imaging MRI Brain with diffusion-weighted imaging (DWI) is the preferred modality: Dermoid cysts typically show fat signal intensity Epidermoid cysts appear with characteristic diffusion restriction CT scan helps identify calcifications and bony remodeling at the skull base Radiological features help differentiate these cysts from other skull base tumors or cystic lesions Clinical Examination Detailed neurological assessment focusing on cranial nerve function Audiological and vestibular tests if applicable Assessment for signs of increased intracranial pressure Treatment Modalities Surgical Management Complete surgical excision is the treatment of choice to relieve mass effect and prevent recurrence Surgery aims to remove the cyst contents and capsule while preserving adjacent neurovascular structures Approaches depend on cyst location: Microsurgical skull base approaches (retrosigmoid, subtemporal, or transnasal endoscopic) Endoscopic techniques increasingly utilized for midline lesions Dr. Nafaur Rahman utilizes advanced microsurgical tools, neuronavigation, and intraoperative monitoring to maximize safety and efficacy in pediatric patients Postoperative Care and Follow-Up Regular MRI scans to monitor for residual cyst or recurrence Rehabilitation for neurological deficits as needed Management of complications such as CSF leaks or infections Prognosis and Outcomes Prognosis is generally excellent with total cyst removal Incomplete excision may lead to recurrence or chemical meningitis Early intervention prevents irreversible neurological damage Long-term follow-up essential due to slow-growing nature and possible recurrence Challenges in Bangladesh Limited pediatric neurosurgical expertise and infrastructure in remote areas Delayed diagnosis due to nonspecific symptoms and lack of awareness Financial and logistic barriers for advanced imaging and surgery Importance of referral to specialized centers like NINS and Bangladesh Paediatric Neurocare Centre for optimal care Why Choose Dr. Md. Nafaur Rahman? Extensive experience in managing rare pediatric skull base cystic lesions Expertise in microsurgical and endoscopic skull base surgery tailored to children Use of modern technology for safer tumor excision and functional preservation Multidisciplinary care including neurology, ENT, radiology, and rehabilitation Compassionate approach focused on improving pediatric patient outcomes in Bangladesh Contact Information Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial & Appointment: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com