Atypical Teratoid Rhabdoid Tumor (AT/RT)
Atypical Teratoid Rhabdoid Tumor (AT/RT)
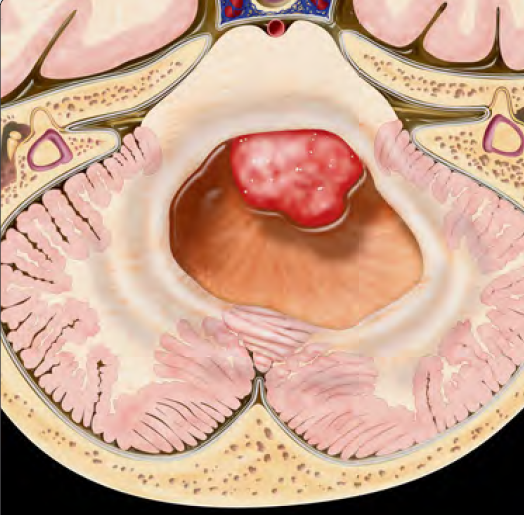
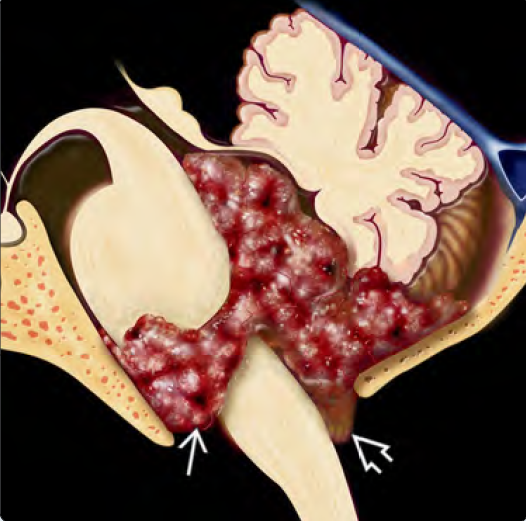
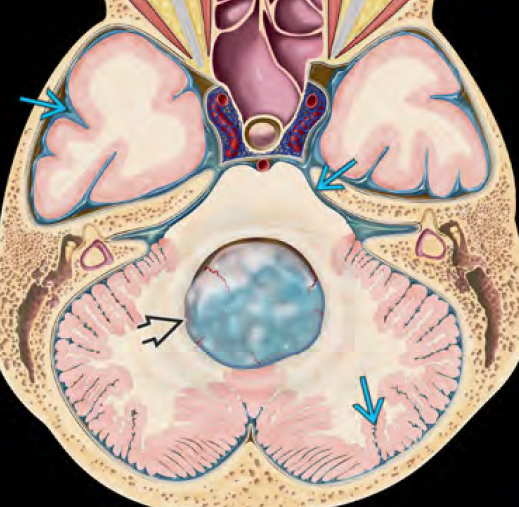
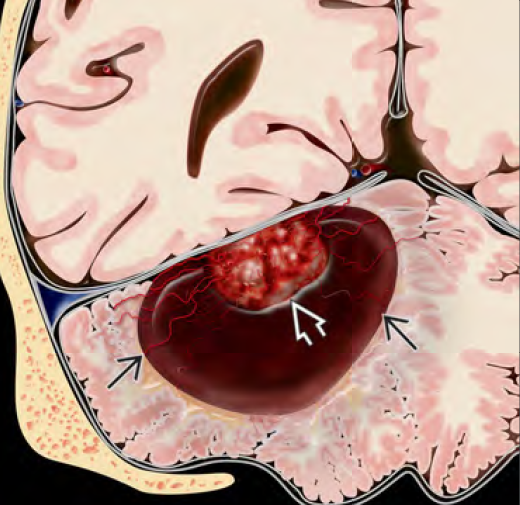
Atypical Teratoid Rhabdoid Tumor (AT/RT) is a rare, highly malignant brain tumor that typically occurs in infants and young children, most commonly under the age of 3 years. It arises in the central nervous system, usually in the posterior fossa (cerebellum or brainstem), but can also be found in the cerebral hemispheres or spinal cord. AT/RT is classified as a World Health Organization (WHO) Grade IV tumor and is distinguished by loss of INI1 (SMARCB1) or SMARCA4 gene mutations, which can be identified through molecular testing. Due to its rapid growth, aggressive nature, and early age of onset, AT/RT is considered one of the most challenging pediatric brain tumors to treat. 🌍 AT/RT in the Bangladesh Context In Bangladesh, awareness of AT/RT is minimal, and children often present with late-stage symptoms due to delays in imaging, lack of specialized pediatric neuro-oncology teams, and resource limitations in pathology and molecular diagnostics. This results in a poor prognosis, despite the potential benefits of early intervention. Dr. Md. Nafaur Rahman, one of Bangladesh’s leading pediatric neurosurgeons, provides comprehensive surgical management for children with AT/RT at the National Institute of Neurosciences & Hospital (NINS) and the Bangladesh Paediatric Neurocare Centre. He collaborates with neuro-oncologists and pediatric intensivists to deliver the best possible care for these complex cases. 🧬 Causes and Genetic Background INI1 gene (SMARCB1) mutation/deletion is a hallmark Can be sporadic or associated with Rhabdoid Tumor Predisposition Syndrome Some cases linked to germline mutations, requiring genetic counseling 🧒 Symptoms of AT/RT in Children Symptoms depend on tumor location and age: Posterior Fossa Tumors (most common): Early morning vomiting and headache Ataxia (unsteady walking) Bulging fontanelle in infants Rapid increase in head size (macrocephaly) Lethargy, feeding difficulty Cranial nerve palsy (facial asymmetry, eye movement problems) Supratentorial Tumors: Seizures Irritability or regression in development Localized weakness or body stiffness In Bangladesh, these symptoms are often overlooked or misdiagnosed as meningitis, gastrointestinal issues, or malnutrition, leading to dangerous diagnostic delays. 🔍 Diagnosis of AT/RT 🧠 MRI Brain with Contrast Typically shows a large, heterogeneous mass with necrosis, hemorrhage, and edema Often crosses midline, may involve ventricles or cause hydrocephalus 🧬 Histopathology with Immunohistochemistry Characterized by rhabdoid cells Loss of INI1 nuclear expression on IHC confirms diagnosis 💉 Lumbar Puncture and CSF Cytology Performed after imaging to assess for CSF dissemination 🧬 Molecular Testing For INI1/SMARCB1 or SMARCA4 gene loss (limited availability in Bangladesh, but feasible in some referral centers) 🛠️ Treatment Strategy for AT/RT AT/RT requires a multidisciplinary approach combining: ✂️ Surgical Resection Maximal safe removal is critical to reduce tumor burden Dr. Nafaur Rahman utilizes advanced microsurgical techniques and intraoperative neuro-navigation to resect tumors while preserving neurological function 💉 Chemotherapy High-dose, multi-agent chemotherapy is essential post-operatively Often given with stem cell rescue (HSCT) in international protocols Local centers in Bangladesh now follow adapted chemotherapy regimens based on international studies ☢️ Radiotherapy Delayed or modified in very young children due to neurotoxicity Used in children >3 years, particularly if gross total resection isn’t achieved 🔄 Prognosis and Survival Poor prognosis overall, especially in children <3 years Median survival ~12–18 months, but longer in patients with complete tumor resection, focal tumors, and older age Ongoing clinical trials exploring targeted therapies (EZH2 inhibitors, immune therapies) ⚠️ Complications if Untreated or Delayed Brainstem compression, leading to coma or death Severe hydrocephalus CSF metastasis and spinal involvement Permanent neurological deficits Failure to thrive and death within months 👨⚕️ Why Choose Dr. Md. Nafaur Rahman? Leading expert in pediatric brain tumors and complex posterior fossa surgeries Offers timely diagnosis, surgical precision, and coordinated oncological care Supported by a multidisciplinary team at NINS and Bangladesh Paediatric Neurocare Centre Trusted by families for ethical, child-centered neurosurgical solutions 📞 Contact for Appointment Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Call for Serial: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com