Pilocytic astrocytoma
Pilocytic astrocytoma
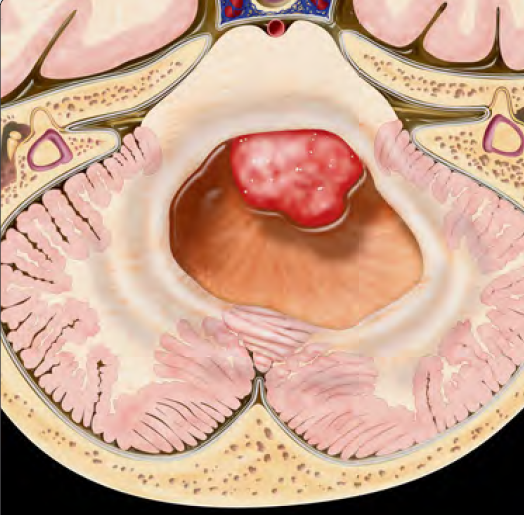
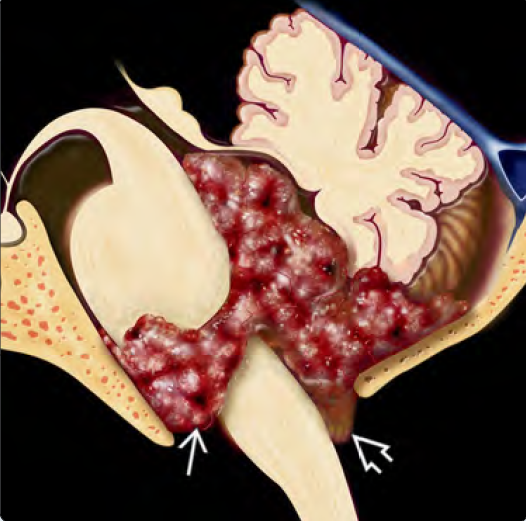
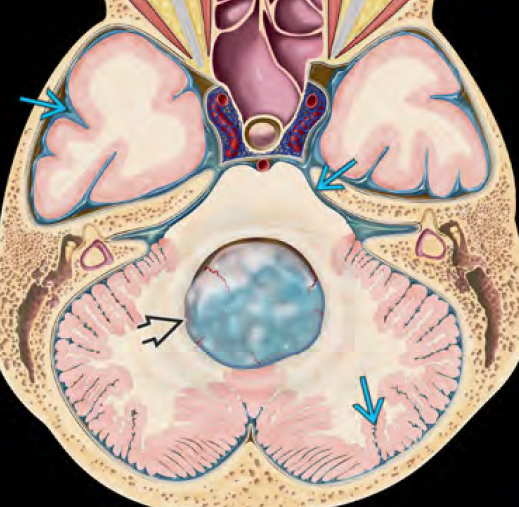
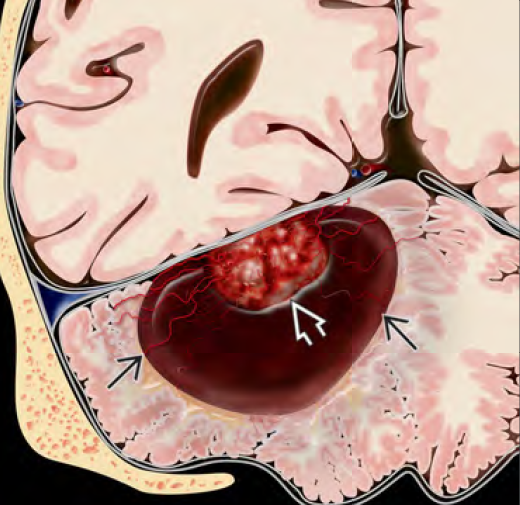
Pilocytic astrocytoma (PA) is a slow-growing, benign (WHO Grade I) brain tumor that originates from astrocytes, the supportive glial cells of the brain. It is the most common primary brain tumor in children, particularly affecting those between 5 to 15 years of age. Unlike malignant tumors, pilocytic astrocytomas rarely invade surrounding tissues and often have an excellent prognosis with complete surgical removal. Most pilocytic astrocytomas arise in the cerebellum (posterior fossa), but they can also occur in the optic pathway, hypothalamus, brainstem, cerebral hemispheres, and spinal cord. 🌍 Pilocytic Astrocytoma in Bangladesh Perspective In Bangladesh, many children with pilocytic astrocytoma present with delayed symptoms due to low awareness, limited access to MRI, and initial misdiagnosis. Parents often consult physicians for recurrent vomiting, imbalance, or visual problems, without considering a brain tumor as a cause. Dr. Md. Nafaur Rahman has extensive experience in diagnosing and surgically treating pilocytic astrocytomas, particularly those located in the cerebellum, brainstem, and optic pathway. He practices at the National Institute of Neurosciences & Hospital (NINS) and offers follow-up care through the Bangladesh Paediatric Neurocare Centre, ensuring safe and effective outcomes for young patients. 🧬 Causes and Pathogenesis Pilocytic astrocytomas are not typically inherited They arise from mutations in the MAPK pathway, including BRAF-KIAA1549 gene fusion Associated with neurofibromatosis type 1 (NF1), especially when involving the optic nerve These tumors grow slowly and often remain localized 🧒 Clinical Symptoms in Children The symptoms depend on the tumor’s location and size: 📍 Cerebellar Tumors (most common): Unsteady gait or frequent falls Headache, especially in the morning Nausea and vomiting Double vision or blurry eyesight Difficulty in coordination 📍 Optic Pathway Tumors: Vision loss or squint Bulging eyes Delayed growth due to hypothalamic involvement 📍 Brainstem Tumors: Facial weakness Swallowing difficulty Nystagmus (eye movement disorder) In Bangladesh, these signs are often attributed to general weakness, sinus infections, or ENT problems, leading to delayed neuroimaging and diagnosis. 🔍 Diagnostic Approach 🧠 MRI Brain with Contrast (Gold Standard) Shows a well-circumscribed, cystic tumor with a mural nodule (classic feature) No significant surrounding edema Often located in the cerebellum or optic pathway Helps plan surgical route and assess CSF obstruction 🔬 Histopathology Confirms WHO Grade I pilocytic astrocytoma Rosenthal fibers and eosinophilic granular bodies are characteristic 🧬 Genetic Testing (when available) BRAF gene fusion studies (not routine in Bangladesh but done in special centers) 🛠️ Treatment of Pilocytic Astrocytoma ✂️ Surgical Resection – Mainstay of Treatment Goal: Total removal of the tumor Dr. Nafaur Rahman performs tumor excision using microsurgical techniques, intraoperative neuromonitoring, and neuro-navigation to avoid damage to vital structures Complete resection usually results in cure without need for chemo or radiotherapy 💧 CSF Diversion (if needed) In cases with hydrocephalus, Endoscopic Third Ventriculostomy (ETV) or VP shunt may be done before or during tumor surgery 💊 Chemotherapy or Radiation (Rarely Needed) Used only for: Incomplete resection Inoperable locations (optic/hypothalamic area) Recurrent tumors 🔄 Prognosis and Recovery Excellent long-term outcome with complete tumor resection 5-year survival > 90% in most cases Majority of children return to normal school and daily life Lifelong cure is possible without recurrence in most patients Some may need vision support, physical therapy, or growth monitoring ⚠️ Risks of Delayed Diagnosis or Incomplete Treatment Progressive neurological disability Permanent visual impairment Obstructive hydrocephalus Brainstem compression, leading to coma or death (rare but critical) Tumor recurrence requiring second surgery 👨⚕️ Why Choose Dr. Md. Nafaur Rahman? Highly experienced in pediatric posterior fossa and optic pathway tumors Performs surgeries with precision, child-safety focus, and minimal complications Treats at Bangladesh’s most advanced neurosurgical facility (NINS) Offers continued care at Bangladesh Paediatric Neurocare Centre, including MRI follow-up, rehab, and neurodevelopmental assessment 📞 Book an Appointment Today Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Serial/Consultation: 01912988182 | 01607033535 🌐 Website: www.neurosurgeonnafaur.com