Ependymoma
Ependymoma
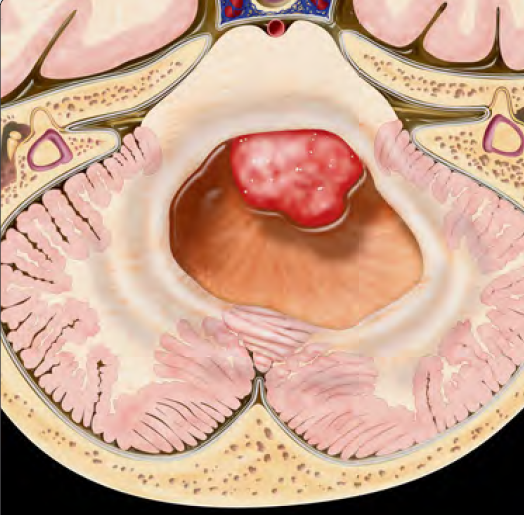
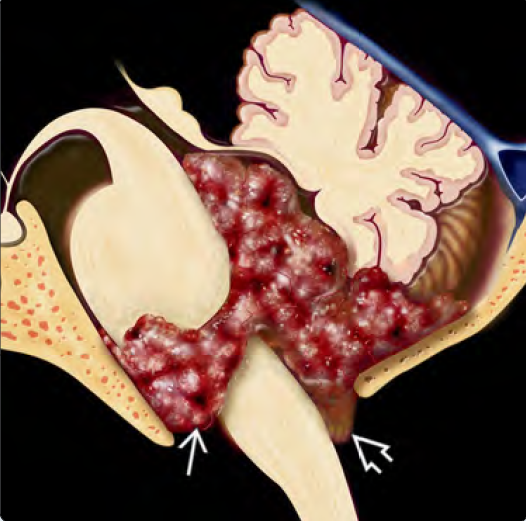
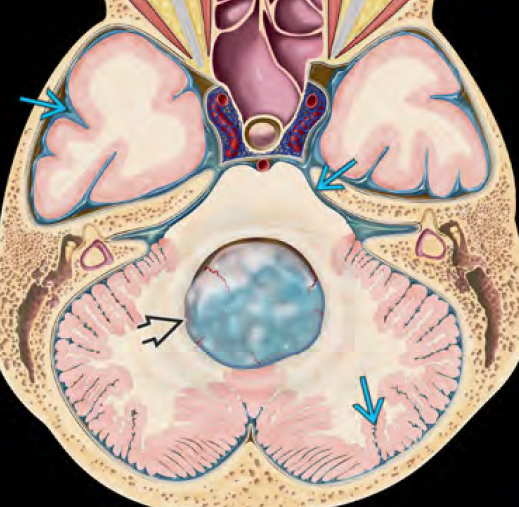
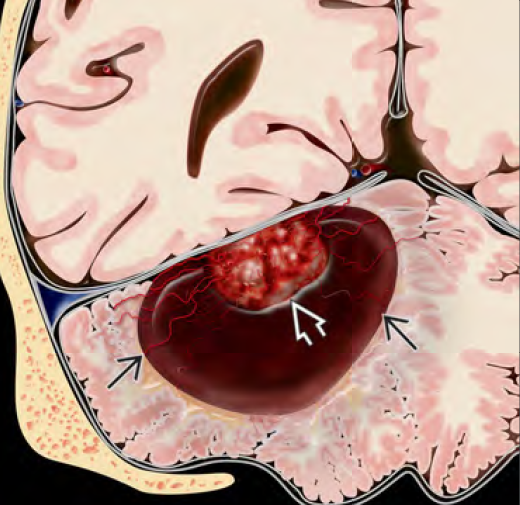
Cranial Ependymoma is a rare malignant brain tumor that arises from the ependymal cells, which line the ventricles (fluid-filled spaces) of the brain and central canal of the spinal cord. In children, it most commonly occurs in the posterior fossa, particularly in the fourth ventricle, causing obstruction of cerebrospinal fluid (CSF) and increased intracranial pressure. Though ependymomas are slow-growing, they can be life-threatening due to their location near critical brain structures. Microsurgical resection, followed by radiotherapy, is the mainstay of treatment. Early intervention significantly improves prognosis, especially when performed by a specialized pediatric neurosurgeon. 🌍 Cranial Ependymoma in Bangladesh: Current Challenges In Bangladesh, awareness about pediatric cranial ependymomas is limited. Children often present late due to misdiagnosis, lack of access to MRI, or treatment from non-specialized centers. This leads to advanced tumor progression, hydrocephalus, and neurological deterioration by the time of proper referral. Dr. Md. Nafaur Rahman, one of Bangladesh’s leading pediatric neurosurgeons, specializes in the complex surgical management of ependymomas, particularly in delicate locations like the posterior fossa. At NINS and Bangladesh Paediatric Neurocare Centre, he ensures safe tumor resection with neuro-monitoring, followed by post-op oncological coordination for holistic care. 🧬 Causes and Risk Factors Most cases are sporadic, with no known environmental or inherited cause Rare associations with neurofibromatosis type 2 (NF2) Genetic mutations like RELA fusion, YAP1 fusion, or ZFTA fusion influence tumor behavior and response to treatment 🧒 Clinical Symptoms in Children Ependymomas often obstruct CSF flow, leading to increased intracranial pressure and symptoms such as: Persistent morning headache Frequent vomiting (especially early morning) Unsteady gait, clumsiness, or frequent falls Double vision, squint, or blurry eyesight Neck stiffness or tilted head posture Developmental regression or irritability in toddlers In advanced cases: lethargy, seizures, or coma In Bangladesh, these symptoms are often confused with gastrointestinal disorders, ear problems, or behavioral issues, delaying the crucial MRI scan. 🔍 Diagnostic Investigations 🧠 MRI Brain with Contrast (Gold Standard) Identifies the exact tumor location, size, and impact on CSF pathways Posterior fossa tumors appear well-defined and heterogeneous, often with cystic components and calcifications 🔍 Spinal MRI Essential to rule out drop metastases via CSF spread 🔬 Histopathology & Molecular Subtyping Confirms diagnosis and helps stratify into risk groups Common types include: Posterior fossa group A (PFA) – common in infants, worse prognosis Posterior fossa group B (PFB) – older children, better prognosis 🛠️ Treatment Plan for Cranial Ependymoma A multidisciplinary, aggressive treatment approach is required: ✂️ Surgical Resection Goal: Maximal safe removal of tumor Dr. Nafaur Rahman uses microsurgical techniques, intraoperative neuromonitoring, and neuro-navigation for high precision Total resection improves long-term survival and reduces recurrence risk Hydrocephalus often improves after tumor excision, avoiding need for permanent CSF diversion 💉 Radiotherapy Recommended after surgery in children above 3 years Targets residual tumor and prevents recurrence Options include focal conformal radiation or proton therapy (not yet available in Bangladesh) 💊 Chemotherapy Limited role; may be considered in incompletely resected tumors, younger children, or clinical trials 🔄 Prognosis & Follow-up Complete resection with radiotherapy offers a 5-year survival of 60–75% in standard-risk children Regular MRI scans, neurological assessments, and rehabilitation are crucial Survivors may need long-term support for learning, coordination, and endocrinological functions ⚠️ Complications if Left Untreated Severe hydrocephalus, leading to brain herniation Permanent neurological deficits (vision loss, motor impairment) Tumor spread to spine Death due to brainstem compression 👨⚕️ Why Choose Dr. Md. Nafaur Rahman? Extensive experience in posterior fossa tumor resection in children Performs surgeries using microsurgical, neuro-monitored, minimally invasive techniques Manages post-op care with dedicated neuro-oncology team Provides holistic support at Bangladesh Paediatric Neurocare Centre Trusted by families across Bangladesh for child-friendly, ethical neurosurgery 📞 Book a Consultation Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Call for Appointment: 01912988182 | 01607033535 🌐 Visit: www.neurosurgeonnafaur.com