Atlantooccipital dislocation (AOD)
Atlantooccipital dislocation (AOD)
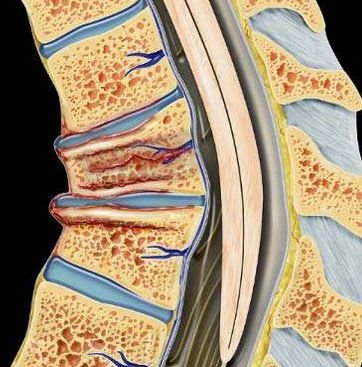
Atlantooccipital dislocation (AOD) is a rare but extremely serious injury where the skull becomes detached from the spine at the junction between the occipital bone (base of the skull) and the first cervical vertebra (atlas or C1). This injury often results from high-velocity trauma, such as car or motorbike accidents, falls from heights, or violent sports injuries. In Bangladesh, where road traffic collisions, construction site falls, and unsafe transport practices are unfortunately common, AOD poses a critical and often fatal threat, particularly to children and young adults. Why AOD is Critical The atlantooccipital joint is responsible for head movement and houses vital structures including the brainstem, spinal cord, cranial nerves, and vertebral arteries. Any dislocation here can lead to immediate respiratory arrest, paralysis, or death. Survivors of AOD usually require urgent neurosurgical intervention, advanced spinal stabilization, and long-term rehabilitation. Timely diagnosis and rapid treatment are essential to prevent fatal outcomes. AOD in the Bangladesh Context In Bangladesh, cases of Atlantooccipital Dislocation often go undetected due to lack of advanced trauma triage, delayed spinal imaging, and limited neurosurgical awareness at primary care centers. Many victims die before reaching a tertiary care facility. However, with increasing access to emergency neuroimaging and spinal surgery—especially at institutions like the National Institute of Neurosciences (NINS)—life-saving interventions are now possible. Dr. Md. Nafaur Rahman is among the very few neurosurgeons in Bangladesh trained in managing high cervical spine trauma, including AOD, especially in pediatric and adolescent populations. Causes of Atlantooccipital Dislocation High-speed road traffic accidents Falls from rooftop, trees, or beds (especially in children) Heavy object trauma to the head/neck Physical abuse or child battering (non-accidental injury) Sports injuries (diving, gymnastics, football) Congenital ligament laxity or connective tissue disorders (rare) Types of Atlantooccipital Dislocation AOD can be classified based on direction of displacement: Anterior Dislocation – Skull shifts forward relative to spine Posterior Dislocation – Skull shifts backward Vertical Dislocation – Skull lifts away vertically (most fatal) Lateral Dislocation – Sideways shift Each type presents unique surgical and neurological challenges and must be urgently identified via imaging. Signs and Symptoms Although many cases are fatal at the scene, patients who survive initial trauma may present with: Neck pain and stiffness Neurological deficits (weakness, numbness, quadriplegia) Difficulty breathing or speaking Loss of consciousness or coma Cranial nerve dysfunction (facial droop, swallowing issues) Unstable or abnormal head posture In children, symptoms may be subtle. Therefore, a high index of suspicion is critical, especially after severe head or neck trauma. Diagnostic Approach in Bangladesh Early detection is key to survival. Dr. Nafaur Rahman recommends an emergency trauma protocol that includes: CT scan with 3D cervical reconstruction – Gold standard for detecting bony displacement MRI cervical spine and brainstem – To assess ligament injury, spinal cord compression, or hemorrhage X-rays (lateral cervical view) – Can show abnormal alignment but may miss subtle dislocations Neurological assessment – Brainstem function, cranial nerves, and consciousness level Special attention is required in pediatric cases, as their flexible ligaments can mask instability on initial imaging. Treatment Strategies AOD is a neurosurgical emergency. Non-operative treatment is rarely sufficient, and immediate stabilization of the craniovertebral junction is essential to save life and function. ✅ Emergency Stabilization Immobilization with cervical collar or halo vest Mechanical ventilation if respiratory centers are compromised Steroids and neuroprotective therapy in selected cases Urgent referral to tertiary neurosurgical center ✅ Definitive Surgical Management Under Dr. Nafaur Rahman’s expert care, surgical intervention includes: Occipito-cervical fusion (OCF) – Gold standard for AOD treatment Use of titanium plates, rods, and screws for rigid fixation Intraoperative neuromonitoring for brainstem safety Microsurgical decompression if spinal cord compression is present Dr. Nafaur uses minimally invasive techniques where possible to minimize blood loss, reduce postoperative complications, and promote quicker recovery. Postoperative Care & Rehabilitation ICU monitoring in the immediate postoperative phase Physiotherapy and spinal precautions for several weeks Speech and swallowing therapy if cranial nerves were affected Psychological support and trauma counseling Return to school or work varies from 6 weeks to 6 months depending on neurological status Prognosis in Bangladesh Outcomes depend heavily on: Time to diagnosis and stabilization Presence of spinal cord or brainstem injury Patient age and overall health Quality of surgical care and rehabilitation With proper management, survival and partial or full neurological recovery is possible. However, delays can result in permanent disability or death. Why Choose Dr. Md. Nafaur Rahman? ✔️ Pioneer in craniovertebral junction surgeries in Bangladesh ✔️ Extensive experience in AOD and AAD management in both children and adults ✔️ Advanced training in spinal instrumentation and fusion techniques ✔️ Works at NINS—Bangladesh’s premier neurosurgery institute ✔️ Compassionate care with individualized rehabilitation planning Book an Emergency Consultation Now 📌 Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📞 Appointment/Serial 📱 +8801912988182 | +8801607033535 🌐 Visit: www.neurosurgeonnafaur.com