Pyogenic Vertebral Osteomyelitis
Pyogenic Vertebral Osteomyelitis
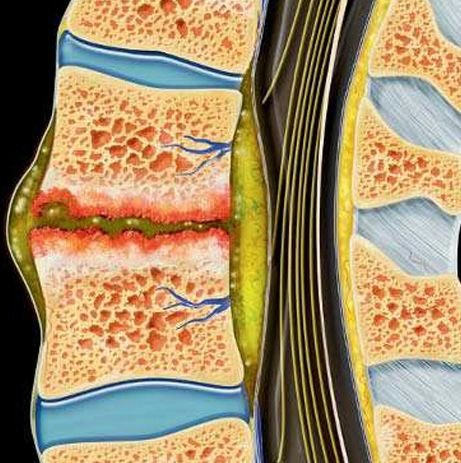
Pediatric Pyogenic Vertebral Osteomyelitis (PVO) is a serious bacterial infection of the vertebral bones in children, most commonly affecting the lumbar and thoracic spine. It may originate from bloodstream infections, trauma, or adjacent soft tissue infections. If not diagnosed and managed promptly, PVO can lead to spinal instability, vertebral collapse, neurological deficits, and even permanent disability. In Bangladesh, late presentation, inadequate early antibiotic use, and limited access to pediatric spinal specialists make this condition more dangerous than in high-resource settings. Dr. Md. Nafaur Rahman specializes in the diagnosis, medical management, and surgical intervention for pediatric vertebral osteomyelitis to ensure safe recovery and full spinal function. 🌍 Burden and Challenges in Bangladesh Infections such as PVO are often underdiagnosed in Bangladesh due to vague symptoms and misinterpretation as simple back pain, growing pains, or muscular strain—especially in young children. Risk factors such as malnutrition, poor hygiene, delayed access to tertiary care, and lack of diagnostic imaging worsen the outcomes. Dr. Nafaur Rahman has treated multiple cases of pediatric spinal infections in children across Bangladesh, offering evidence-based and child-centric care, including advanced imaging, long-term antibiotics, and minimally invasive spinal surgery when required. ⚠️ Signs and Symptoms of Pediatric Vertebral Osteomyelitis Symptoms can be subtle in children, especially infants and toddlers, and should be carefully interpreted: 🧍 Severe or persistent back pain, worse with movement 🛏️ Reluctance or refusal to sit, walk, or stand 🌡️ Low-grade or persistent fever 🧒 Irritability, malaise, or difficulty sleeping 🦠 Localized spinal tenderness or deformity 🧑🦽 Neurological symptoms like numbness, weakness, or bladder dysfunction in advanced stages 🩺 Abnormal posture, limping, or bent back (kyphotic deformity) “When back pain and fever coexist in a child, vertebral osteomyelitis must be considered, especially in areas with limited healthcare access.” — Dr. Md. Nafaur Rahman 🧬 Causes and Pathogens Most cases are caused by hematogenous spread of bacteria to the spine. Common organisms include: Staphylococcus aureus – most frequent cause Streptococcus species Gram-negative bacteria – E. coli, Pseudomonas Mycobacterium tuberculosis – must be ruled out in endemic areas like Bangladesh Rarely, fungal or mixed infections in immunocompromised children 🧪 Diagnostic Investigations Dr. Nafaur Rahman follows a stepwise diagnostic protocol to ensure early and precise diagnosis: 🧲 MRI Spine with contrast – The most sensitive imaging tool 📸 X-Ray and CT scan – For bone destruction and deformity in later stages 🧪 Blood tests – ESR, CRP, CBC (usually elevated) 🩸 Blood culture – Identifies causative organism in ~50% of cases 💉 CT-guided biopsy or aspiration – For microbiological and histopathological confirmation 🧫 Tuberculosis screening – Mantoux test, GeneXpert, chest X-ray in suspected TB osteomyelitis 🛠️ Treatment of Pediatric Pyogenic Vertebral Osteomyelitis 💊 Medical Management: Initial treatment is conservative unless complications develop: Hospital admission for bed rest and IV antibiotics Broad-spectrum antibiotics followed by targeted therapy (4–6 weeks IV + oral) Analgesics and anti-inflammatory medications Bracing for spinal support and comfort Monitoring with serial ESR/CRP and repeat imaging 🧠 Surgical Intervention (Indicated in): Spinal cord compression with neurological signs Vertebral collapse causing spinal deformity Persistent abscess or failure of medical therapy Instability requiring spinal fusion or decompression Dr. Nafaur Rahman performs: Spinal decompression and drainage of abscess Microdiscectomy or corpectomy in severe destruction Stabilization with pediatric spinal implants Minimally invasive approaches where feasible to reduce recovery time “Surgery is crucial not only to treat infection but to preserve spinal alignment and neurological function in growing children.” — Dr. Md. Nafaur Rahman 🔁 Recovery and Follow-Up Care Recovery is usually excellent if treatment is timely. Dr. Nafaur Rahman’s care protocol includes: 📅 Regular follow-up imaging (MRI or X-ray) 💉 Repeat blood markers to monitor inflammation 🧒 Pediatric physiotherapy for mobility and posture correction 🧠 Psychological support for school reintegration and confidence rebuilding 🩺 Nutritional and immunity-boosting guidance for long-term wellness 🚨 Potential Complications If Untreated 🧠 Permanent spinal deformity (kyphosis or scoliosis) ⚡ Paralysis or nerve damage 🧑🦽 Bladder or bowel dysfunction 💀 Sepsis or systemic infection 🛌 Chronic pain or mobility limitation 👨⚕️ Why Trust Dr. Md. Nafaur Rahman for Pediatric Spinal Infections? 🏥 Leading neurosurgeon in pediatric spinal infection and deformity correction in Bangladesh 🧠 Performs advanced spine surgery with precision and safety 🔬 Emphasizes early diagnosis and infection control 👨👩👧 Cares for each child with a multidisciplinary approach including pediatrics, ID, nutrition, and rehab 🌟 Trusted across Bangladesh for managing complex pediatric spinal conditions 📞 Contact Dr. Nafaur Rahman for Expert Evaluation and Treatment Dr. Md. Nafaur Rahman Assistant Professor, Pediatric Neurosurgery, National Institute of Neurosciences & Hospital (NINS) Chief Consultant, Bangladesh Paediatric Neurocare Centre 📱 For Serial/Appointments: 📞 01912988182 | 📞 01607033535 🌐 Visit: www.neurosurgeonnafaur.com
YouTube Videos and Patient Reviews on Pyogenic Vertebral Osteomyelitis